
1.
Introduction
Lymph node dissection (LND) has either an established or
increasingly recognized oncologic role in several genitouri-
nary malignancies, including penile, bladder, and prostate
cancer
[1–3]. However, its role in the management of renal
cell carcinoma (RCC) is controversial. Although LND
improves staging, its impact on oncologic outcomes is
unclear. The only randomized trial of LND reported no
survival benefit in low-risk patients
[4]. Still, retrospective
data suggest a potential oncologic benefit in patients at
increased risk of nodal metastases
[5–13]. Accordingly, US
and European guidelines suggest LND in patients with
clinical lymphadenopathy
[14,15].
Given the uncertainty regarding the therapeutic role of
LND, the purpose of this study was two-fold. First, we
evaluated the association of LND with oncologic outcomes
among a large cohort of patients undergoing radical
nephrectomy (RN) for RCC using a propensity score (PS)-
based approach. Second, we attempted to identify which
high-risk patient populations may benefit from LND.
2.
Patients and methods
2.1.
Patient population
After obtaining Institutional Review Board approval, we identified
1797 patients who underwent RN for sporadic, unilateral, M0 RCC
between 1990 and 2010 at the Mayo Clinic. Of these, 606 (34%)
underwent concurrent LND. The decision to perform LND was at the
surgeon’s discretion, and a standardized template was not employed
throughout the study time frame.
2.2.
Clinicopathologic and radiographic features
Clinicopathologic features recorded included year of surgery, age at
surgery, sex, symptoms at presentation, smoking status, Eastern
Cooperative Oncology Group performance status, Charlson score, body
mass index, receipt of neoadjuvant therapy, surgical approach (open or
laparoscopic), pathologic tumor size, RCC histologic subtype, stage
according to the 2010 American Joint Committee on Cancer classifica-
tion, grade according to the World Health Organization/International
Society of Urologic Pathologists classification, and presence of coagu-
lative tumor necrosis or sarcomatoid differentiation. All pathology slides
were rereviewed by one urologic pathologist (J.C.C.). In addition,
preoperative radiographic features were recorded frommedical records,
including lymphadenopathy on computed tomography (CT; cN1), renal
vein involvement on CT or magnetic resonance imaging, inferior vena
cava involvement on CT or magnetic resonance imaging, and radio-
graphic evidence of hemorrhage, necrosis, calcification, extrarenal
extension, neovascularity, adrenal involvement, or cystic or indetermi-
nate cysts.
2.3.
Statistical methods
Clinicopathologic and radiographic features were summarized with
medians/interquartile ranges (IQRs) and frequency counts/percentages,
and compared by receipt of LND using Wilcoxon rank sum, chi-square,
and Fisher exact tests. PSs for receipt of LND were obtained using a
logistic regression model with LND as the outcome and the features
listed in
Table 1as covariates, with the exception of body mass index and
neoadjuvant treatment, as described in the Supplementary data
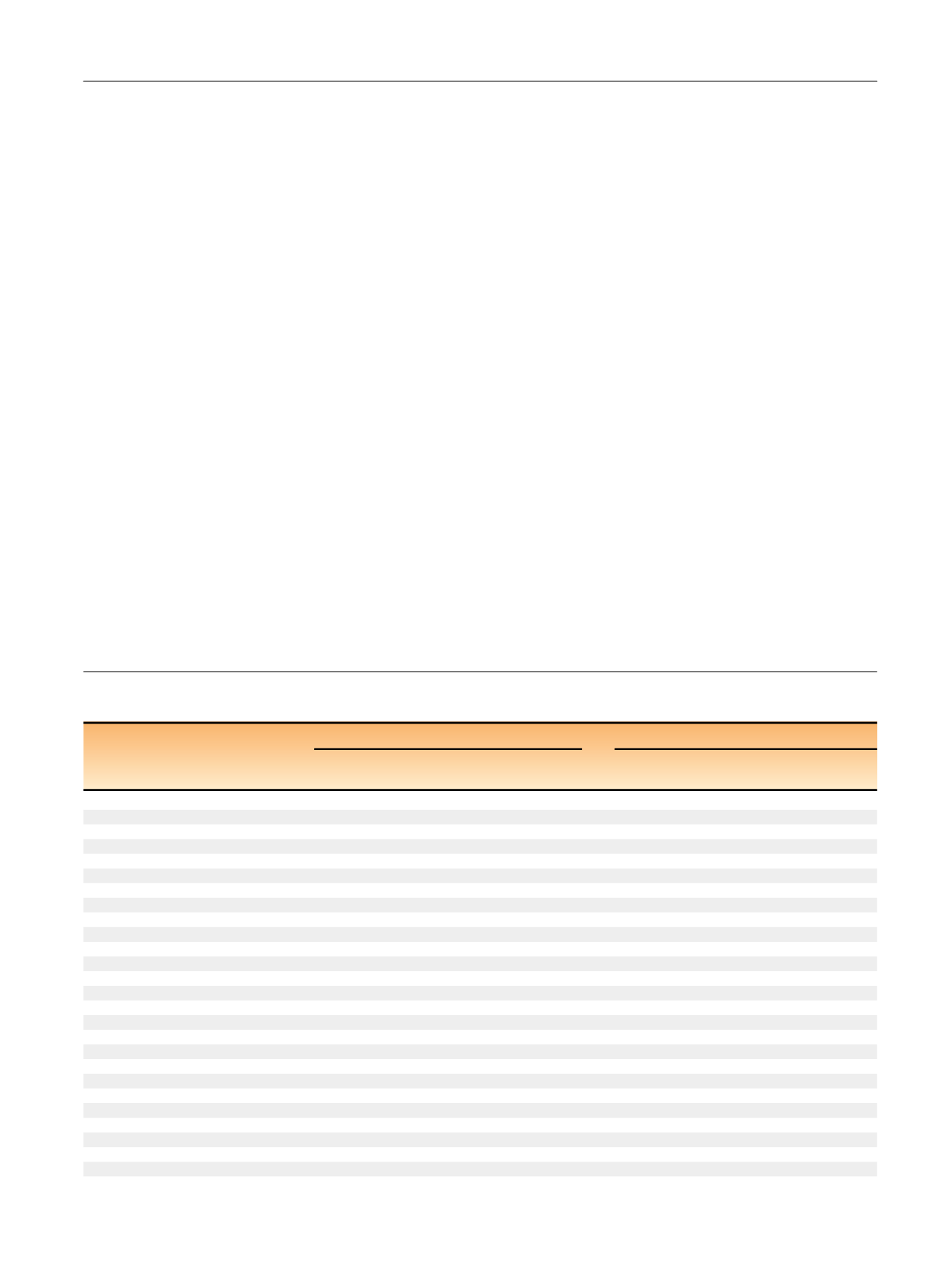
Table 1 – Clinicopathologic and radiographic features stratified by receipt of lymph node dissection (LND) in the original cohort (
N
= 1797)
and in the pseudo cohort obtained after adjustment by inverse probability weights (
N
= 1637)
Original cohort (
N
= 1797)
Pseudo cohort (
N
= 1637)
No LND
(
N
= 1191)
LND
(
N
= 606)
p
value
No LND
(
N
= 1102)
LND
(
N
= 535)
p
value
Feature
Median (IQR)
Median (IQR)
Charlson score (
N
= 1768)
1 (0–2)
0 (0–2)
<
0.001
1 (0–2)
0 (0–2)
0.80
BMI (kg/m
2
;
N
= 1650)
28 (25–32)
28 (25–32)
0.67
28 (25–32)
28 (25–31)
0.43
Tumor size (cm;
N
= 1789)
5.5 (3.9–8.0)
9.4 (7.0–12.0)
<
0.001
6.6 (4.5–9.0)
6.7 (4.7–9.5)
0.85
Year of surgery
N
(%)
<
0.001
N
(%)
[20_TD$DIFF]
0.55
1990–1994
334 (28)
96 (16)
276 (25)
136 (25)
[1_TD$DIFF]
1995–1999
314 (26)
103 (17)
[2_TD$DIFF]
278 (25)
143 (27)
2000–2004
319 (27)
164 (27)
297 (27)
142 (27)
2005–2010
224 (19)
243 (40)
251 (23)
114 (21)
Age at surgery (yr)
[21_TD$DIFF]
<
0.001
0.82
18–54
263 (22)
169 (28)
263 (24)
133 (25)
55–64
289 (24)
171 (28)
[2_TD$DIFF]
272 (25)
123 (23)
[3_TD$DIFF]
65–74
383 (32)
179 (30)
364 (33)
172 (32)
75
256 (21)
87 (14)
203 (18)
107 (20)
Sex
[22_TD$DIFF]
0.40
0.97
Female
415 (35)
199 (33)
[4_TD$DIFF]
389 (35)
189 (35)
[5_TD$DIFF]
Male
776 (65)
407 (67)
713 (65)
346 (65)
Symptoms (
N
= 1795)
646 (54)
459 (76)
<
0.001
672 (61)
324 (61)
0.91
Constitutional symptoms (
N
= 1795)
218 (18)
188 (31)
<
0.001
241 (22)
118 (22)
0.96
Smoking status (
N
= 1769)
[23_TD$DIFF]
0.02
0.72
Never
517 (44)
242 (41)
488 (44)
248 (46)
Current
182 (16)
125 (21)
[6_TD$DIFF]
180 (16)
84 (16)
[7_TD$DIFF]
Former
473 (40)
230 (39)
434 (39)
203 (38)
ECOG performance status (
N
= 1796)
[24_TD$DIFF]
0.56
0.67
0
1,015 (85)
522 (86)
961 (87)
470 (88)
1
133 (11)
61 (10)
[8_TD$DIFF]
102 (9)
48 (9)
[9_TD$DIFF]
2
22 (2)
14 (2)
19 (2)
7 (1)
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 5 6 0 – 5 6 7
561
















