
inferior vena cava
[25]. In addition, some efferent lymphatic
vessels may drain directly into the thoracic duct, bypassing
the retroperitoneal LNs
[25] .Consequently, RCC may be less
likely to have a prolonged loco-regional phase than other
genitourinary malignancies, and enhanced local control in
the retroperitoneum may therefore not translate into a
survival benefit.
However, other explanations exist. LND may be associat-
ed with a small oncologic benefit that the present study may
not have detected. It is also possible that LND is associated
with improved survival for a high-risk patient subset that we
did not examine. Furthermore, it is possible that salvage
therapies, such as salvage surgery or earlier administration
of systemic therapy for retroperitoneal recurrence, may have
mitigated the impact of LND at the time of RN
[28] .In
addition, application of a risk-adapted approach to LND may
have resulted in apparent reverse causation. Indeed, we
observed a modestly increased risk of distant metastases
using adjustment for PS quintile and stratification by PS
quintile, which may reflect reverse causation, residual
unmeasured confounding, or chance given multiple statisti-
cal comparisons. However, there was no evidence of reverse
causation with regard to CSM or ACM.
This study is limited by its retrospective and nonran-
domized design. Importantly, neither the decision to
perform LND nor the extent of LND was standardized.
Furthermore, the experience of an academic center may not
be generalizable to other settings, and these results require
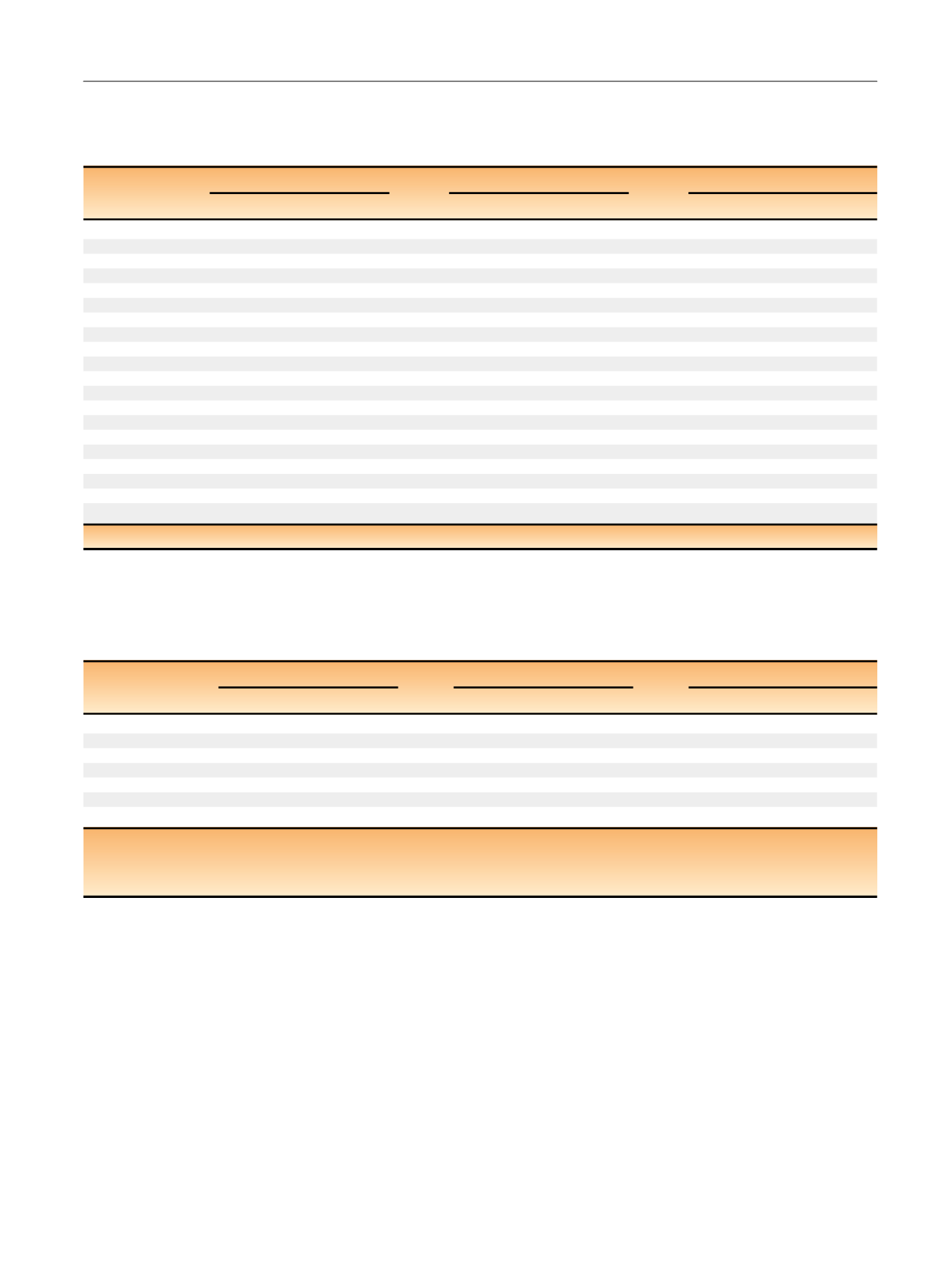
Table 4 – Association of number of lymph nodes (LNs) removed (continuous) with oncologic outcomes among patients who underwent LN
dissection (
N
= 590). Hazard ratio (HR) represents the association of a 10-LN increase in the number of LNs removed with the outcome of
interest, except for the cN1/pN0 subset, where it represents the association of
I
13 versus <13 LNs removed with the outcome of interest
(HR > 1 indicates increased risk of event)
Distant metastases
CSM
ACM
HR (95% CI)
p
value
HR (95% CI)
p
value
HR (95% CI)
p
value
Univariable
All
1.23 (1.09–1.39)
0.001
1.06 (0.91–1.23)
0.47
1.11 (0.98–1.26)
0.11
cN0/pN0
1.10 (0.90–1.35)
0.34
0.83 (0.62–1.12)
0.22
1.06 (0.87–1.29)
0.58
cN0/pN1
0.83 (0.50–1.37)
0.47
0.70 (0.41–1.20)
0.19
0.68 (0.41–1.12)
0.13
cN1/pN0
1.1
1 a[19_TD$DIFF]
(0.54–2.25)
0.78
1.0
9 a (0.52–2.27)
0.82
1.0
9 a (0.56–2.13)
0.80
cN1/pN1
1.03 (0.81–1.31)
0.81
0.99 (0.75–1.32)
0.95
1.07 (0.83–1.39)
0.59
Multivariabl
e b0.96 (0.83–1.12)
0.59
0.84 (0.71–1.01)
0.07
0.98 (0.84–1.13)
0.74
ACM = all-cause mortality; CI = confidence interval; CSM = cancer-specific mortality.
a
Given evidence of a nonlinear association, HR represents 13 versus
<
13 LNs removed with the outcome of interest.
b
Adjusted for year of surgery, age at surgery, sex, symptoms at presentation, smoking status, Eastern Cooperative Oncology Group performance score, Charlson
score, cN, surgical approach, tumor size, histologic subtype, pT stage, pN stage, and grade.
Table 3 – Association of lymph node dissection (LND) with the development of distant metastases, cancer-specific mortality (CSM), or all-
cause mortality (ACM) among patients at increased risk of pN1 disease. Models included an indicator for LND, and indicator for risk of pN1
disease (eg, cN1 or threshold probability), and the interaction term between the two. Hazard ratios (HRs) and
p
values represent LND versus
no LND (HR > 1 indicates increased risk of event)
Distant metastases
CSM
ACM
Risk group
HR (95% CI)
p
value
HR (95% CI)
p
value
HR (95% CI)
p
value
Adjusted for PS quintile
cN1
0.71 (0.33–1.54)
0.39
0.94 (0.41–2.15)
0.88
0.86 (0.41–1.78)
0.68
Risk of pN1
0.05
1.29 (1.04–1.60)
0.02
1.15 (0.91–1.46)
0.23
1.11 (0.92–1.34)
0.27
0.10
1.20 (0.93–1.54)
0.16
1.04 (0.80–1.36)
0.78
1.08 (0.86–1.35)
0.51
0.15
1.28 (0.98–1.67)
0.08
1.11 (0.83–1.47)
0.48
1.07 (0.85–1.36)
0.57
0.20
1.11 (0.71–1.72)
0.65
1.05 (0.67–1.64)
0.82
1.04 (0.70–1.54)
0.85
0.30
0.75 (0.45–1.24)
0.26
0.75 (0.45–1.27)
0.28
0.73 (0.46–1.17)
0.19
0.40
1.06 (0.41–2.75)
0.90
1.19 (0.46–3.06)
0.72
0.86 (0.38–1.96)
0.72
0.50
1.07 (0.40–2.82)
0.90
1.23 (0.47–3.23)
0.67
0.86 (0.37–1.98)
0.72
IPW
cN1
0.75 (0.38–1.46)
0.40
0.94 (0.46–1.92)
0.86
0.86 (0.46–1.64)
0.65
Risk of pN1
0.05
1.12 (0.91–1.36)
0.29
0.97 (0.78–1.21)
0.79
0.96 (0.81–1.14)
0.65
0.10
1.16 (0.92–1.46)
0.21
1.02 (0.79–1.31)
0.89
1.01 (0.82–1.24)
0.94
0.15
1.31 (1.02–1.68)
0.04
1.13 (0.87–1.48)
0.37
1.05 (0.84–1.32)
0.66
0.20
1.11 (0.73–1.70)
0.63
1.05 (0.68–1.61)
0.82
0.99 (0.67–1.46)
0.95
0.30
1.03 (0.63–1.68)
0.92
1.03 (0.62–1.70)
0.91
0.86 (0.53–1.38)
0.52
0.40
1.21 (0.60–2.47)
0.60
1.22 (0.60–2.47)
0.58
0.98 (0.51–1.91)
0.96
0.50
1.23 (0.57–2.65)
0.60
1.25 (0.59–2.66)
0.56
0.98 (0.48–2.00)
0.95
CI = confidence interval; IPW = inverse probability weights; PS = propensity score.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 5 6 0 – 5 6 7
565
















