
 [16]
[16]
. Forty-six patients were excluded from PS calculation due to missing
data (14 with and 32 without LND), and 110 had a PS that did not fall
within the common range (69 with and 41 without LND). A total of
1641 patients formed the cohort for PS analysis, including 523 (32%) who
underwent LND. Sixty-four patients were missing the cause of death
(16 with and 48 without LND) and were therefore excluded from
analyses of cancer-specific mortality (CSM). For PS matching, there were
153 patients who underwent LND (including 40 cN1 patients and
57 with predicted probability of pN1 0.20) for whom suitable matched
pairs could not be found as described in the Supplementary data, leaving
370 matched pairs for analysis.
The associations of LND with the development of distant metastases,
CSM, and all-cause mortality (ACM) were evaluated with Cox models
using several PS techniques, and summarized with hazard ratios (HRs)
and 95% confidence intervals (CIs). PS techniques included 1:1 PS
matching (
n
= 370 matched pairs), adjustment for PS quintile, stratifica-
tion by PS quintile, and reweighting using stabilized inverse probability
weights (IPWs) as described in the Supplementary data. HRs for
stratified analyses were obtained by pooling estimates obtained within
each PS quintile, and HRs for the subset of 370 matched pairs were
obtained by stratifying on the matched sets. In models further adjusted
for the surgeon, similar results were obtained (data not shown). To
incorporate patients excluded from PS analysis, we also performed
traditional Cox multivariable regression for the 1751 patients with
nonmissing data, adjusting for all covariates used to estimate the PS.
Reasoning that patients at increased risk of LN metastases may
particularly benefit from LND, we conducted several analyses to further
evaluate the association of LND with oncologic outcomes among
patients at increased risk of pN1 disease. To do so, we constructed
Cox models, adjusted using PS techniques, which included an indicator
for LND, an indicator for risk of pN1 disease, and the interaction term
between the two. We considered patients with preoperative radio-
graphic lymphadenopathy (cN1) as well as patients with threshold
probabilities for pN1 disease ranging from 0.05 to 0.50 at increased risk of
pN1 disease. Predicted probabilities for pN1 disease were estimated by
constructing amultivariable logistic regressionmodel fromthe 606 patients
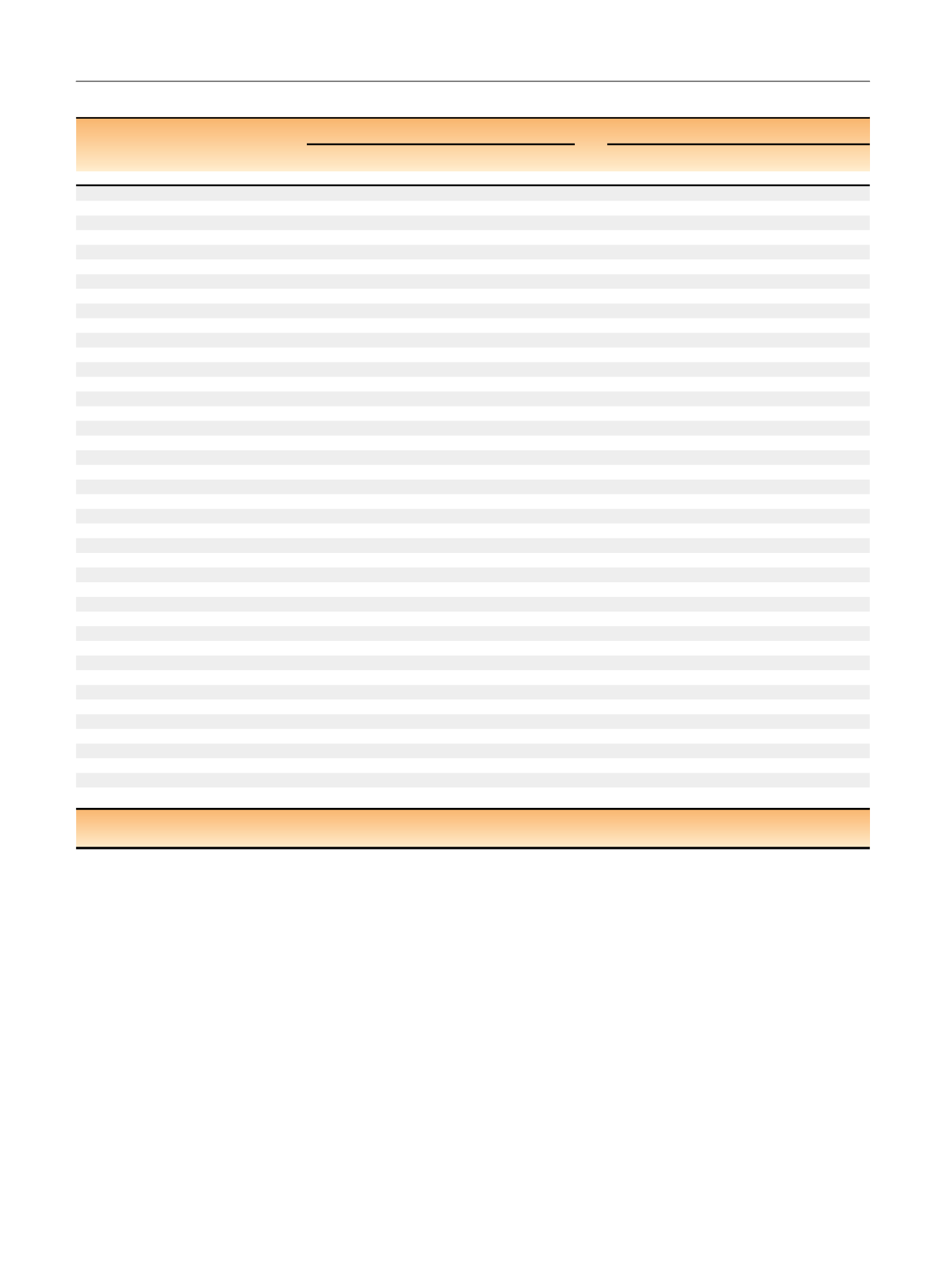
Table 1 (
Continued
)
Original cohort (
N
= 1797)
Pseudo cohort (
N
= 1637)
No LND
(
N
= 1191)
LND
(
N
= 606)
p
value
No LND
(
N
= 1102)
LND
(
N
= 535)
p
value
3
18 (2)
8 (1)
18 (2)
10 (2)
4
3 (
<
1)
0
2 (
<
1)
0
cN1
11 (1)
108 (18)
<
0.001
37 (3)
18 (3)
0.96
Renal vein involvement on CT/MRI
87 (7)
189 (31)
<
0.001
147 (13)
71 (13)
0.94
IVC tumor thrombus on CT/MRI
56 (5)
117 (19)
<
0.001
98 (9)
45 (8)
0.77
Radiographic evidence of:
Hemorrhage
24 (2)
15 (2)
0.53
28 (3)
17 (3)
0.40
Necrosis
71 (6)
91 (15)
<
0.001
101 (9)
52 (10)
0.74
Calcification
76 (6)
65 (11)
0.001
81 (7)
44 (8)
0.57
Extrarenal extension
32 (3)
90 (15)
<
0.001
51 (5)
26 (5)
0.81
Neovascularity
71 (6)
99 (16)
<
0.001
87 (8)
40 (7)
0.79
Adrenal involvement
8 (1)
7 (1)
0.29
6 (1)
4 (1)
0.58
Cystic or indeterminate cysts
254 (21)
78 (13)
<
0.001
197 (18)
102 (19)
0.53
Neoadjuvant treatment
0
4 (1)
0.01
0
1 (
<
1)
0.13
Type of surgery
[25_TD$DIFF]
<
0.001
0.57
Open radical nephrectomy
1,005 (84)
569 (94)
[2_TD$DIFF]
967 (88)
475 (89)
[10_TD$DIFF]
Laparoscopic radical nephrectomy
186 (16)
37 (6)
135 (12)
60 (11)
RCC histologic subtype
[26_TD$DIFF]
0.006
0.27
Clear cell
942 (79)
507 (84)
885 (80)
428 (80)
Papillary
162 (14)
49 (8)
[11_TD$DIFF]
127 (12)
66 (12)
[12_TD$DIFF]
Chromophobe
68 (6)
35 (6)
65 (6)
33 (6)
Collecting duct
2 (
<
1)
5 (1)
2 (
<
1)
3 (1)
Not otherwise specified
13 (1)
6 (1)
18 (2)
2 (
<
1)
Mucinous tubular and spindle cell
1 (
<
1)
0
1 (
<
1)
0
Translocation-associated
[13_TD$DIFF]
1 (
<
1)
0
1 (
<
1)
0
[27_TD$DIFF]
Clear cell papillary
2 (
<
1)
4 (1)
3 (
<
1)
3 (1)
2010 pT (
N
= 1785)
[28_TD$DIFF]
<
0.001
0.79
pT1a
340 (29)
36 (6)
222 (20)
106 (20)
pT1b
352 (30)
84 (14)
[2_TD$DIFF]
293 (27)
151 (28)
[14_TD$DIFF]
pT2a
152 (13)
81 (13)
153 (14)
70 (13)
pT2b
65 (6)
66 (11)
76 (7)
36 (7)
pT3a
210 (18)
218 (36)
253 (23)
123 (23)
pT3b
41 (3)
91 (15)
71 (6)
34 (6)
pT3c
11 (1)
13 (2)
17 (2)
8 (1)
pT4
9 (1)
16 (3)
17 (2)
7 (1)
Grade
[29_TD$DIFF]
<
0.001
0.27
1
75 (6)
12 (2)
57 (5)
22 (4)
2
590 (50)
154 (25)
[2_TD$DIFF]
465 (42)
218 (41)
[12_TD$DIFF]
3
460 (39)
310 (51)
487 (44)
246 (46)
4
66 (6)
130 (21)
93 (8)
49 (9)
Coagulative tumor necrosis (
N
= 1796)
309 (26)
308 (51)
<
0.001
351 (32)
182 (34)
0.36
Sarcomatoid differentiation
29 (2)
42 (7)
<
0.001
35 (3)
20 (4)
0.53
BMI = body mass index; CT = computed tomography; ECOG = Eastern Cooperative Oncology Group; IQR = interquartile range; MRI = magnetic resonance
imaging; RCC = renal cell carcinoma.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 5 6 0 – 5 6 7
562
















