
94.3–100%), FP rate 0% (IQR 0–5.0%), and FN rate 4.8% (IQR
0–18.2%;
Table 2).
3.5.
Sensitivity analyses
In 19 studies, ePLND was used as a reference standard.
Sensitivity analyses for these 19 studies showed median
sensitivity of 95.2% (IQR 85.6–100%) and a FN rate of 4.8%
(IQR 0–14.5%), similar to the overall percentage for all
studies (Supplementary Table 1). When we analyzed SNB
performed only for intermediate-risk and high-risk prostate
cancers in 13 studies, lower median sensitivity (94.3%, IQR
83.7–100%) and a higher FN rate were observed (5.8%, IQR
0–16.3%; Supplementary Table 2). When we excluded
studies with high RoB
[17,19,30,36] ,DTA outcome param-
eters did not change significantly (Supplementary Table 3).
The median percentage of LN-positive patients with only
metastases in SN(s) was 72.9% (IQR 56.6–100%). Finally,
sensitivity analysis was performed for patients with LN
metastases found outside the ePLND template, regardless of
whether ePLNDwas positive or negative; the median FP rate
increased to 4.9% (IQR 0–10.2%) with sensitivity of 95.7%
(IQR 86.1–100%).
3.6.
Effect of different definitions of SN on outcomes
The studies included used different definitions of SNs in PCa.
Eight studies
[21,24,27–31,33]followed the SN definition of
SN introduced by Wawroschek et al
[37] ,who stated that all
preoperatively and intraoperatively identified radioactive
LNs would be defined as the SN (Definition 1). Two studies
[23,26]defined the SN(s) as the first node(s) that accumu-
lated radiocolloids on early (15 min) lymphoscintigrams
and/or nodes detected on late (2–3 h) lymphoscintigrams
(and/or SPECT CT imaging) in the same regions that were not
seen on early images (Definition 2). Six other studies
[17– 20,22,32]considered all radiocolloid-containing LNs with a
node-to-background count density ratio higher than 2 in
vivo and greater than 10 counts/s ex vivo as SNs (Definition
3). Four studies that used intraoperative ICG fluorescence
imaging
[16,25,35,36]defined every fluorescent LN as an SN
(Definition 4). These different definitions and the use of
tracers with different properties influenced the number of
SNs resected. This was also reflected in the outcome
parameters. Definition 2 showed lower median sensitivity
of 87.5% and a higher FN rate of 12.5%, but a higher FP rate of
3.2%. The highest number of SNs was resected for Definition
4, leading to sensitivity of 100%, with an FN rate 0% and FP
rate of 0%. These results were consistent with the type of
tracer. A summary of the results by definition and tracer are
shown in Supplementary Tables 4 and 5.
3.7.
Discussion
3.7.1.
Principal findings
To the best of our knowledge, this is the first systematic
review addressing the diagnostic performance of SNB in
nodal staging of PCa, taking into account the different
definitions of SN and using standardized diagnostic
accuracy definitions. First, using data from 21 studies, we
found an estimated overall median sensitivity of 95.2%,
which is promising and appears to be nearly twice as high as
the average sensitivity reported for
11
C- and
18
F-choline-
and
68
Ga-PSMA PET/CT
[2,3]. Second, the median rate of
histologically positive SNs outside the ePLND template
when the dissection template was negative (ie, FP rate) was
0%. This suggests that in addition to ePLND, SNB does not
provide any additional benefit over and above ePLND in
terms of identifying nodal disease outside the dissection
template at patient level.
Crucially, the review identified significant heterogeneity
in terms of how DTA outcomes for SNB were reported in the
literature. In particular, there is confusion regarding the role
of ePLND as reference standard. For instance, true positive
cases should be those in whom histologically positive LNs
were identified within the ePLND template, either by ePLND
or SNB. Even in cases in which SNB identified histologically
positive nodes within the ePLND template, but subsequent
ePLND did not reveal any positive nodes, such patients
should be classed as true positives. False positives are cases
for which the ePLND was negative while SNB identified
histologically positive nodes outside ePLND template. In
other words, if only ePLND had been performed, these
additional positive cases would have been undetected and
such patients would be incorrectly staged as pN0. Although
it appears counterintuitive, the reason these cases are
termed FP is because all diagnostic accuracy measures must
be calculated based on the results of the reference standard
(ie, ePLND) as denominator. Consequently, a high FP value
(or low specificity, because FP = 1 – specificity) reflects the
inadequacy of ePLND as a staging procedure, and better
nodal staging by SNB compared to ePLND.
3.7.2.
Implications for clinical practice and further research
3.7.2.1. Diagnostic value.
The review revealed that the diag-
nostic accuracy of SNB is almost comparable to that of
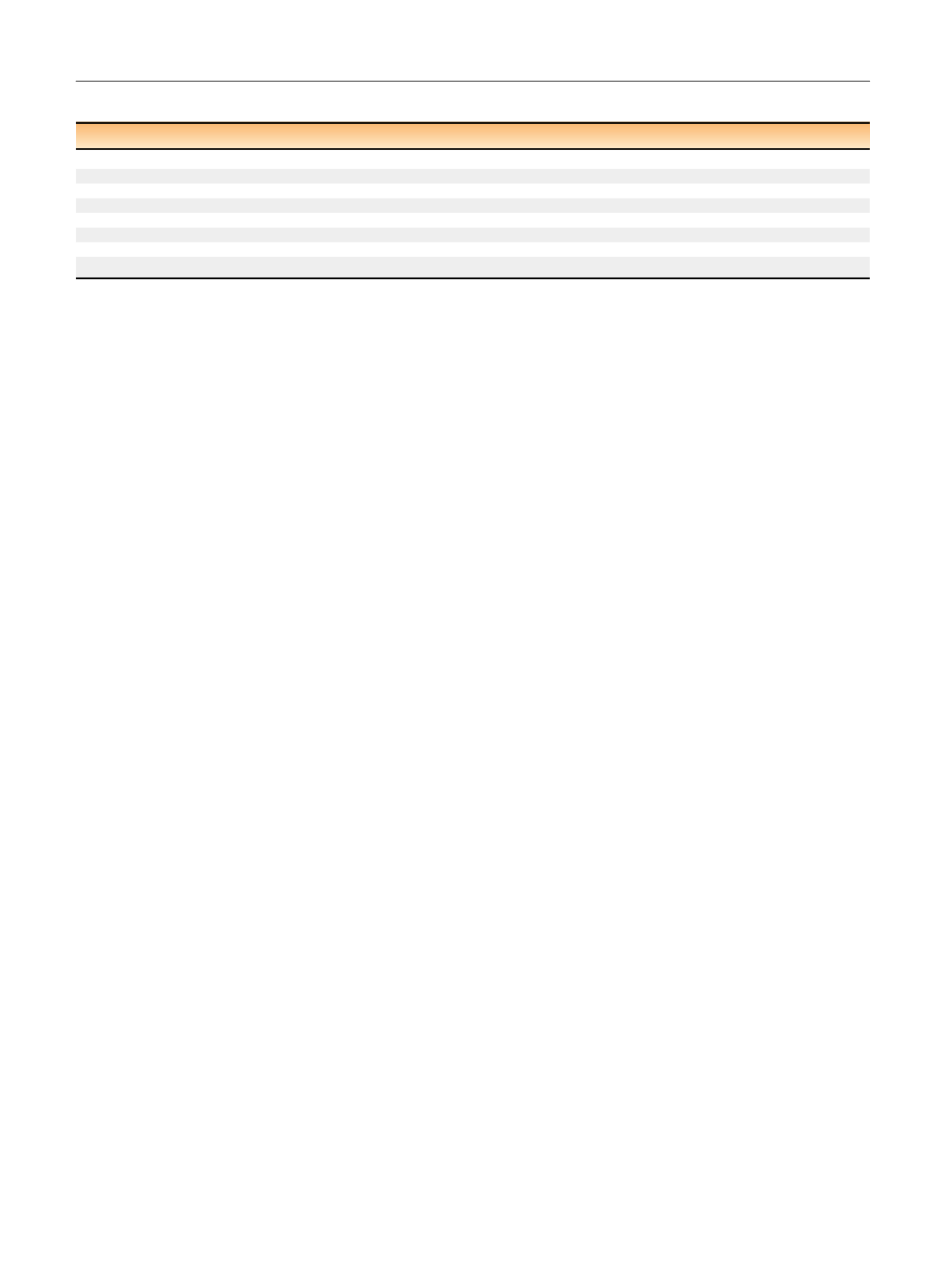
Table 2 – Overall diagnostic test accuracy for all the studies included in the review
Median
Interquartile range
Minimum
Maximum
Diagnostic yield (%)
95.9
89.4–98.5
76.0
100
Nondiagnostic rate (%)
4.1
1.5-10.7
0
24.0
Sensitivity (%)
95.2
81.8-100
50.0
100
Specificity (%)
100
95.0–100
91.7
100
Positive predictive value (%)
100
87.0–100
50.0
100
Negative predictive value (%)
98.0
94.3–100
81.4
100
False positive rate (%)
0
0–5.0
0
8.3
False negative rate (%)
4.8
0–18.2
0
50.0
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 5 9 6 – 6 0 5
602
















