
postimplantation incontinence and urinary morbidity. ED
develops in about 40% of the patients after 3–5 yr.
High-dose rate (HDR) brachytherapy uses a radioactive
source temporarily introduced into the prostate to deliver
radiation. HDR brachytherapy can be delivered in single or
multiple fractions and is often combined with EBRT of at
least 45 Gy as a method of dose escalation in intermediate-
or high-risk PCa. Quality-of-life changes are similar to high-
dose EBRT alone
[87] .HDR brachytherapy as monotherapy
has been pioneered in a small number of centres with low
published toxicity and high biochemical control rates but
currently mature data are not available on the optimal
treatment schedule
[88].
12.
Alternative local treatment options
Besides RP, EBRT, and brachytherapy, other modalities have
emerged as therapeutic options in patients with clinically
localised PCa. However patients with a life expectancy
>
10
yr should be fully informed that there are limited data on
the long-term outcome for cancer control beyond 10 yr.
Recently, focal therapy has been developed, with the aim to
ablate tumours selectively while sparing the neurovascular
bundles, sphincter, and urethra. Based on the available data
[89], it should still be considered as fully experimental.
Cryosurgery might be considered for patients with an
organ-confined PCa or minimal tumour extension beyond
the prostate, prostate volumes
<
40 ml, PSA
<
20 ng/ml, and
GS
<
7.
A systematic review compared cryotherapy versus RP
and EBRT
[89]. Data from 3995 patients across 19 studies
were included. In the short term, there was conflicting
evidence relating to cancer-specific outcomes. The 1-yr
disease-free survival was worse for cryotherapy than for
either EBRT or RP. None of the other cancer-specific
outcomes including OS showed any significant differences.
The high risk of bias across studies precludes any clear
conclusions.
High-intensity focussed ultrasound (HIFU) of the
prostate was compared in a systematic review
[89]with RP and EBRT as primary treatment for localised
PCa. Data from 4000 patients across 21 studies were
included. HIFU had a significantly worse disease-free
survival at 1 yr compared with EBRT. The differences
were no longer significant at 3 yr. The biochemical result
was in contrast to OS at 4 yr, which was higher when
using HIFU. The quality of the evidence was poor, due to
high risks of bias across studies precluding any clear
conclusion. The overall PCa
[8_TD$DIFF]
Guidelines are summarised in
Table 8.
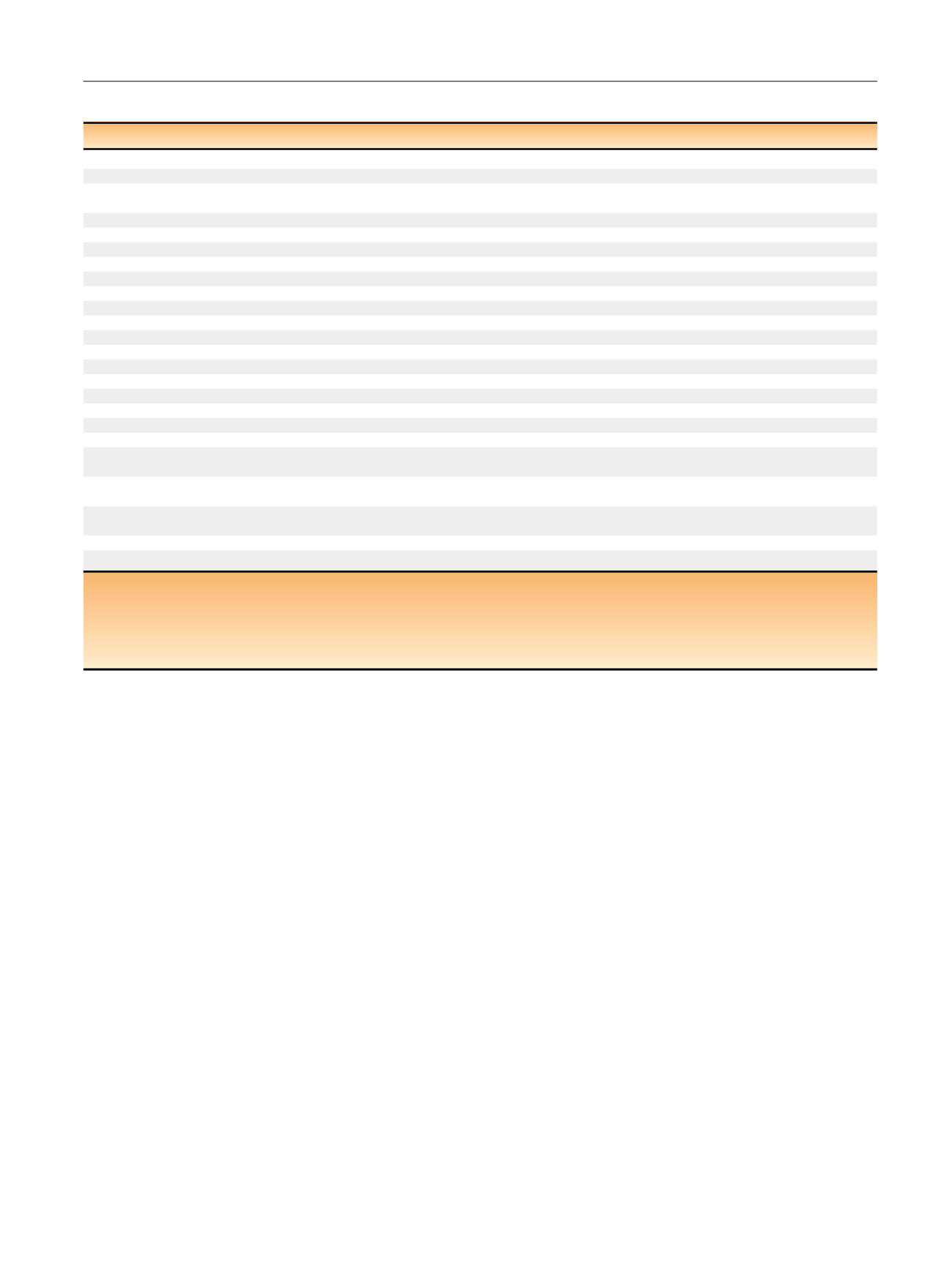
Table 8 – Summary of the main findings regarding treatment of nonmetastatic prostate cancer
Recommendation
LE
GR
Management decisions should be made after all treatments have been discussed in a multidisciplinary team
4
A *Offer RP to patients with low- and intermediate-risk PCa and a life expectancy
>
10 yr
1b
A
Nerve-sparing surgery may be attempted in preoperatively potent patients with low risk for extracapsular disease
(T1c, GS
<
7, and PSA
<
10 ng/ml, or refer to Partin tables/nomograms)
2b
B
In intermediate- and high-risk disease, use mpMRI as a decision tool to select patients for nerve-sparing procedures
2b
B
Offer RP in a multimodality setting to patients with high-risk localised PCa and a life expectancy
>
10 yr
2a
A
Offer RP in a multimodality setting to selected patients with locally advanced (cT3a) PCa and a life expectancy
>
10 yr
2b
B
Offer RP in a multimodality setting to highly selected patients with locally advanced PCa (cT3b–4 N0 or any T N1)
3
C
Do not offer NHT before RP
1a
A
Do not offer adjuvant HT for pN0
1a
A
Offer adjuvant ADT for node positive (pN+)
1b
A
Offer EBRT using IMRT to all risk groups
2a
A
In patients with low-risk PCa, without a previous TURP, with a good IPSS and a prostate volume
<
50 ml, offer LDR brachytherapy
2a
A
In low risk PCa, use a total dose of 74–78 Gy
1a
A
In intermediate- risk PCa use a total dose of 76–78 Gy, in combination with short-term ADT (4–6 mo)
1b
A
In patients with high-risk localised PCa, use a total dose of 76–78 Gy in combination with long-term ADT (2–3 yr)
1b
A
In patients with locally advanced cN0 PCa, offer radiation therapy in combination with long-term ADT (2–3 yr)
1a
A
In patients with cN1 PCa, offer pelvic external irradiation in combination with immediate long-term ADT
2b
B
Offer adjuvant ADT for pN1 after ePLND
1b
A
Discuss adjuvant ADT with additional radiation therapy for pN1 after ePLND
2b
A
Offer observation (expectant management) for pN1 after ePLND when two or fewer nodes show microscopic involvement with a
PSA
<
0.1 ng/ml and absence of extranodal extension
2b
B
In patients with pT3N0M0 PCa and an undetectable PSA following RP, discuss adjuvant EBRT because it at least improves
biochemical-free survival
1a
A
Inform patients with pT3N0M0 PCa and an undetectable PSA following RP about salvage irradiation as an alternative to adjuvant
irradiation when PSA increases
2b
A
Only offer cryotherapy and HIFU within a clinical trial
3
B
Do not offer focal therapy of the prostate outside a clinical trial
3
A
ADT = androgen-deprivation therapy; EBRT = external beam radiation therapy; ePLND = extended pelvic lymph node dissection; GR = grade of
recommendation; GS = Gleason score; HIFU = high-intensity focussed ultrasound; HT = hormone therapy; IMRT = intensity-modulated radiation therapy;
IPSS = International Prostate Symptom Score; LDR = low-dose rate; LE = level of evidence; mpMRI = multiparametric magnetic resonance imaging;
NHT = neoadjuvant hormone therapy; PCa = prostate cancer; PSA = prostate-specific antigen; RP = radical prostatectomy; TURP = transurethral resection of
the prostate.
*
Upgraded following Panel consensus.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 6 1 8 – 6 2 9
625
















