
7.
Primary local treatment
Management decisions should be made after all options
have been discussed with a multidisciplinary team (includ-
ing urologists, radiation oncologists, medical oncologists,
pathologists, and radiologists), and after the balance of
benefits and side effects of each therapy modality has been
considered together with the patient.
8.
Active surveillance and watchful waiting
Active surveillance (AS) aims to reduce overtreatment in
men with very low-risk PCa, without compromising
opportunities for cure, whereas watchful waiting (WW) is
a conservative management for frail patients until the
possible development of clinical progression leading to
symptomatic treatment. The major differences between
these two modalities are detailed in
Table 7.
Mortality from untreated screen-detected PCa in
patients with GS 5–7 can be as low as 7% at 15 yr follow-
up
[37] .An RCT was unable to show an OS and CSS
difference at 10 yr between RP and WW in 731 men with
screen-detected clinically organ-confined PCa
[38]. Only
patients with intermediate risk or with a PSA
>
10 ng/ml
had a significant OS benefit from RP (hazard ratio [HR]:
0.69 [0.49–0.98] and 0.67 [0.48–0.94], respectively). A
population-based analysis in 19 639 patients aged 65 yr
who were not given curative treatment found that in men
having a Charlson Comorbidity Index score 2, tumour
aggressiveness had little impact on OS at 10 yr
[39]. These
data highlight the potential role of WW in some patients
with an individual life expectancy
<
10 yr.
A systematic review summarised the available data on
AS
[40]. There is considerable variation between studies
regarding patient selection, follow-up policies, and when
active treatment should be instigated. Selection criteria for
AS include clinical T1c or T2a, PSA
<
10 ng/ml, and PSA
density
<
0.15 ng/ml per ml (even if still controversial
[41]),
fewer than two to three positive cores with
<
50% cancer
involvement of every positive core, GS 6. Extraprostatic
extension or lymphovascular invasion should not be
considered for AS
[42]. Rebiopsy to exclude Gleason
sampling error is considered important
[41], and mpMRI
has a major role based on its high NPV value for lesion
upgrading and to exclude anterior prostate lesions
[43] .Fol-
low-up in AS is based on repeat biopsy
[41], serial PSA
measurements, and DRE, the optimal schedule remaining
unclear. Strategies how to incorporate mpMRI within this
follow-up are evolving but are not yet established. The
decision to switch to an active treatment is based on a
change in the inclusion criteria (T stage and biopsy results).
The use of a PSA change (especially a PSA doubling time
<
3
yr) remains contentious based on its weak link with grade
progression. Active treatment may also be triggered upon a
patient’s request
[44].
9.
Radical prostatectomy
The goal of RP is eradication of PCa while preserving
continence and, whenever possible, potency. It is the only
treatment for localised PCa to show a benefit for OS and CSS,
compared with WW. Patients should not be denied this
procedure on the grounds of age alone
[21]provided they
have at least 10 yr of life expectancy and are aware that
increasing age is linked to increased incontinence risk.
Nerve-sparing RP can be performed safely in most men with
localised PCa. High risk of extracapsular disease, such as any
cT2c or cT3 or any GS
>
7, are usual contraindications. An
externally validated nomogram predicting side-specific
extracapsular extension can help guide decision making
[45]. mpMRI may be helpful for selecting a nerve-sparing
approach because it has good specificity (0.91; 95% CI, 0.88–
0.93) but low sensitivity (0.57; 95% CI, 0.49–0.64) for
detecting microscopic pT3a stages
[46]. But the experience
of the radiologist remains of paramount importance.
Lower rates of positive surgical margins for high-volume
surgeons suggest that experience and careful attention to
surgical details can improve surgical cancer control
[47]and
lower the complication rate.
There is still no evidence that one surgical approach is
better than another (open, laparoscopic, or robotic), as
highlighted in a formal systematic review. Robot-assisted
prostatectomy is associated with lower perioperative
morbidity and a reduced positive margins rate compared
with laparoscopic prostatectomy, although there is consid-
erable methodological uncertainty. No formal differences
exist in cancer-related continence or erectile dysfunction
outcomes
[48].
9.1.
Pelvic lymph node dissection
The individual risk of finding positive lymph nodes can be
estimated using externally validated preoperative nomo-
grams such as that described by Briganti
[49]. A risk of nodal
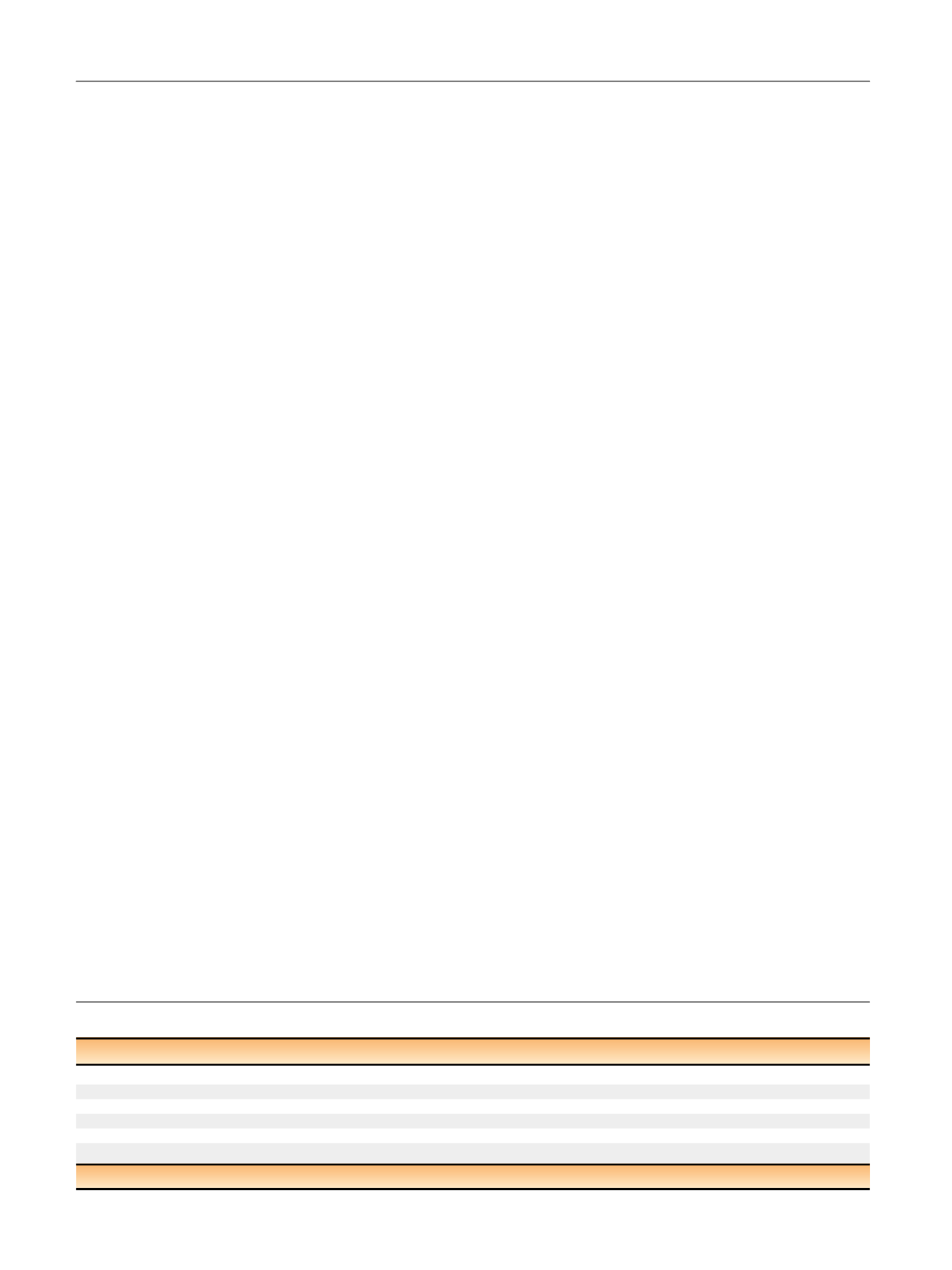
Table 7 – Definitions of active surveillance and watchful waiting
Active surveillance
Watchful waiting
Treatment intent
Curative
Palliative
Follow-up
Predefined schedule
Patient specific
Assessment/Markers used
DRE, PSA, rebiopsy, mpMRI
Not predefined
Life expectancy
>
10 yr
<
10 yr
Aim
Minimise treatment-related toxicity without compromising survival
Minimise treatment-related toxicity
Comments
Only for low-risk patients
Can apply to patients at all stages
DRE = digital rectal examination; PSA = prostate-specific antigen; mpMRI = multiparametric magnetic resonance imaging.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 6 1 8 – 6 2 9
622
















