
predominant mixed UI, and no high-grade prolapse),
performing urodynamics does not improve surgical
outcome. However, currently there is no better test to
evaluate bladder function than urodynamic or videour-
odynamic testing, and in patients with complicated UI and
those who do not respond to first-line therapies, urody-
namics may provide valuable information that can guide
management and improve both patient and physician
confidence in prescribed therapies.
Conflicts of interest:
Gary E. Lemack is a stock shareholder of Pfizer, a
company consultant for Medtronic, has received company speaker
honoraria from Astellas and Allergan, and is a trial participant for
Sophiris. The remaining authors have nothing to disclose.
Acknowledgments:
The authors would like to thank the other members
of the EAU Urinary Incontinence guideline panel for their comments and
suggestions: Mr. M. Lucas, Prof. A. Tubaro, Prof. F. Cruz, Prof. J.L.H.R.
Bosch, and Mr. N. Thiruchelvam. We would also like to thank Miss Karin
Plass and the other members of the EAU Guidelines Office team for their
ongoing efforts and support.
References
[1]
Davis DM. The hydrodynamics of the upper urinary tract (urody- namics). Ann Surg 1954;140:839–49,[6_TD$DIFF]
PMCID: PMC1609699.[2] Haylen BT, de Ridder D, Freeman RM, et al. IUGA/ICS joint report on
the terminology for female pelvic floor dysfunction. Neurourol Uro-
dyn 2010;29:4–20
. http://dx.doi.org/10.1002/nau.20798 .[3] Winters JC, Dmochowski RR, Goldman HB, et al. Urodynamic studies
in adults: AUA/SUFU guideline. J Urol 2012;188:2464–72
. http://dx. doi.org/[7_TD$DIFF]
10.1016/j.juro.2012.09.081 .[4] National Institute for Health and Care Excellence. Urinary inconti-
nence in women: management. NICE guideline CG171. NICE; 2013.
[5] Burkhard FC, Lucas MG, Berghmans LC, et al. EAU guidelines on urinary
incontinence. Arnhem The Netherlands: European Association of
Urology 2016
[8_TD$DIFF]
http://uroweb.org/guideline/urinary-incontinence/[6] Nager CW, Brubaker L, Litman HJ, et al. A randomized trial of urody-
namic testing before stress-incontinence surgery. N Engl J Med
2012;366:1987–97
. http://dx.doi.org/10.1056/NEJMoa1113595.
[7] van Leijsen SAL, Kluivers KB, Mol BW, et al. Value of urodynamics
before stress urinary incontinence surgery: a randomized controlled
trial. Obstet Gynecol 2013;121:999–1008
. http://dx.doi.org/[
9
_
T
D
$
D
I
F
F
]
10. 1097/AOG.0b013e31828c68e3 .[8] Brostrom S, Jennum P, Lose G. Short-term reproducibility of cysto-
metry and pressure-flow micturition studies in healthy women.
Neurourol Urodyn 2002;21:457
. http://dx.doi.org/[
1
0
_
T
D
$
D
I
F
F
]
10.1002/nau. 10019 .[9] Clement KD, Lapitan MCM, Omar MI, Glazener CMA. Urodynamic
studies for management of urinary incontinence in children and
adults. Cochrane Database Syst Rev 2013;2013:CD003195
. http://dx. doi.org/10.1002/14651858.CD003195.pub3 .[(Fig._1)TD$FIG]
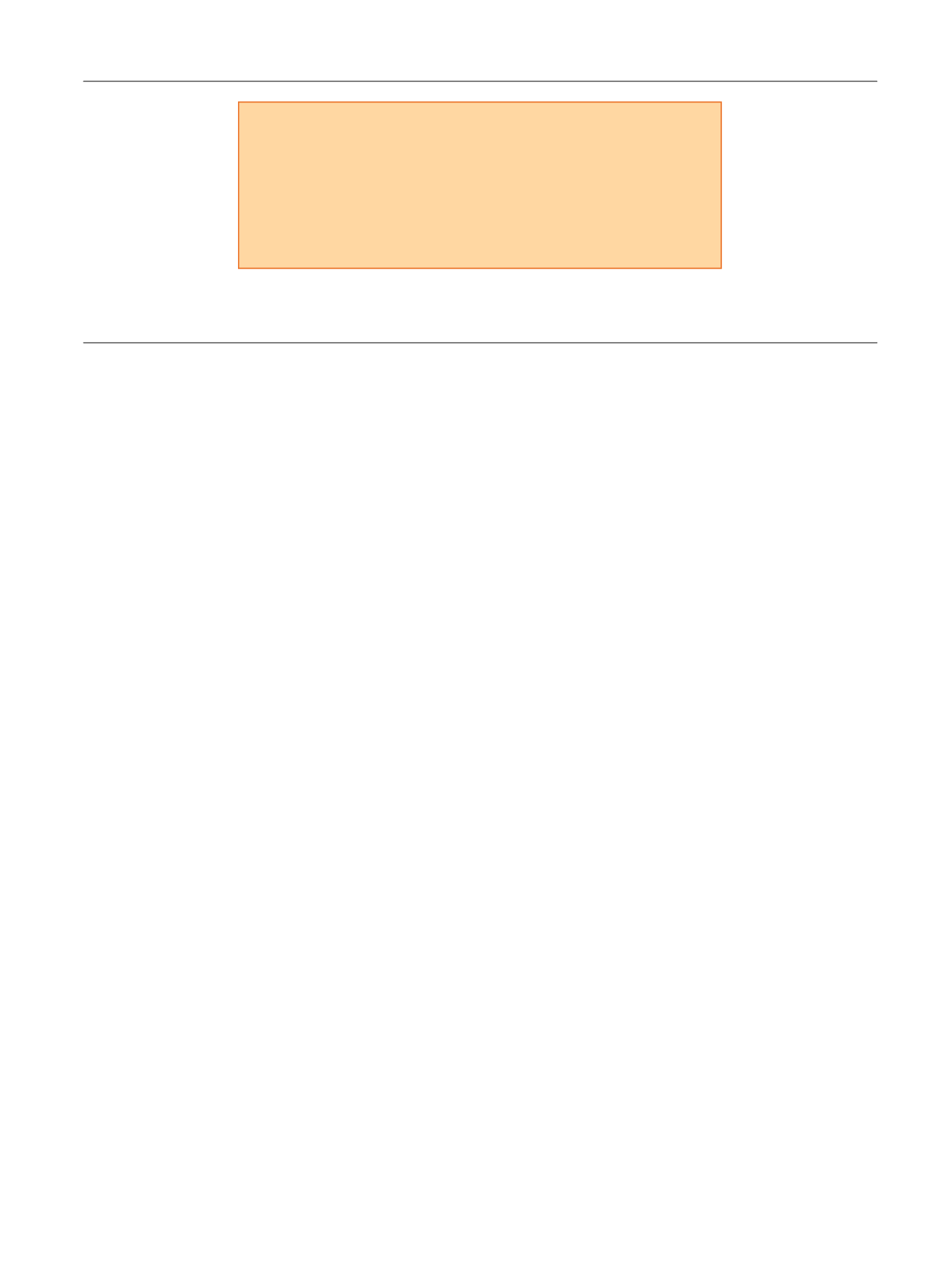
Complicated urinary incontinence
•
UI associated with genitourinary prolapse
•
Mixed UI (equally bothersome stress and urgency UI)
•
Previous surgery for UI
•
Neurogenic bladder dysfunction
•
UI associated with known structural abnormality of the urinary tract
•
Continuous UI (suspected ϐistula or urethral diverticulum)
Fig. 1 – What is meant by
complicated urinary incontinence
. Repeated reference is made in the text to uncomplicated urinary incontinence (UI), so it is
useful to clarify what is meant by complicated UI, and by extension the type of cases for which urodynamics may be of significant benefit.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 5 0 1 – 5 0 3
503
















