
The direct comparison of MRI-GB and TRUS-GB within
the same population demonstrates that there is no
statistically significant difference for overall PCa detection.
Though a per core analysis demonstrates a statistically
significant increased incidence of PCa in target biopsy cores
when compared with systematic biopsy cores, with a
relative yield of 3.91 (95% CI: 3.17–4.83). When focussing on
the detection of csPCa MRI-GB has a statistically significant
advantage over TRUS-GB, with a relative sensitivity of
1.16 (95% CI: 1.02–1.32), indicating that MRI-GB signifi-
cantly detects more clinically significant cancers than
TRUS-GB. Consequently, MRI-GB has a statistically signifi-
cant lower yield of insignificant PCa compared with TRUS-
GB, with a relative yield of 0.47 (95% CI: 0.35–0.63). These
results support MRI-GB as a superior alternative to TRUS-
GB. These findings are similar to findings of a previous
meta-analysis comparing TRUS-GB to MRI-GB in which the
authors found a relative sensitivity for MRI-GB of 1.05 (95%
CI: 0.94–1.19) for overall PCa, and a relative sensitivity of
1.20 (95% CI: 1.09–1.32) for csPCa
[41].
Are we ready to abandon systematic TRUS-GB and
completely replace it for MRI-GB? Based on this meta-
analysis, omitting TRUS-GB would result in missing 19% of
all PCa cases, and 10% of csPCa cases. Simultaneously, by
omitting TRUS-GB 50% of the insignificant PCa would not be
detected and would thereby decrease overdiagnosis of
these tumours. The debate on whether this is acceptable or
not is ongoing and a definite conclusion is beyond the scope
of this review.
Which technique for MRI-GB should then be preferred?
The results of this current meta-analysis indicate that
MRI-TB has an advantage over COG-TB in overall PCa
detection (
p
= 0.02). There does not seem to be a significant
advantage of MRI-TB compared with FUS-TB, or FUS-TB
compared with COG-TB for overall PCa detection. When
focussing on the detection of csPCa, there does not seem to
be a significant advantage of any particular technique,
though the number of studies used for this specific meta-
analysis was limited. When comparing various techniques
of MRI-GB essential components are targeted lesion
characteristics, such as PI-RADS classification, lesion size,
and lesion location. Of 43 included studies only 5% (
n
= 2)
presented data regarding lesion diameter, and 58% (
n
= 25)
applied PI-RADS classification. Furthermore the applied
threshold for target biopsy will directly impact the found
tumour yield, and as mentioned earlier the included studies
demonstrate significant heterogeneity regarding applied
threshold. Consequently the results of this meta-analysis are
indicative at best: the number of randomised controlled
trials directly comparing one technique with another is
limited. Within the cohort presented in this meta-analysis
there were only two studies directly comparing two
techniques
[34,42]. Both studies were not able to demon-
strate significant differences between COG-TB and FUS-TB
on overall cancer and clinically significant cancer detection.
Although a multivariate analysis in one study demonstrated
increased cancer detection in smaller MRI lesions using
FUS-TB when directly compared with COG-TB
[42].
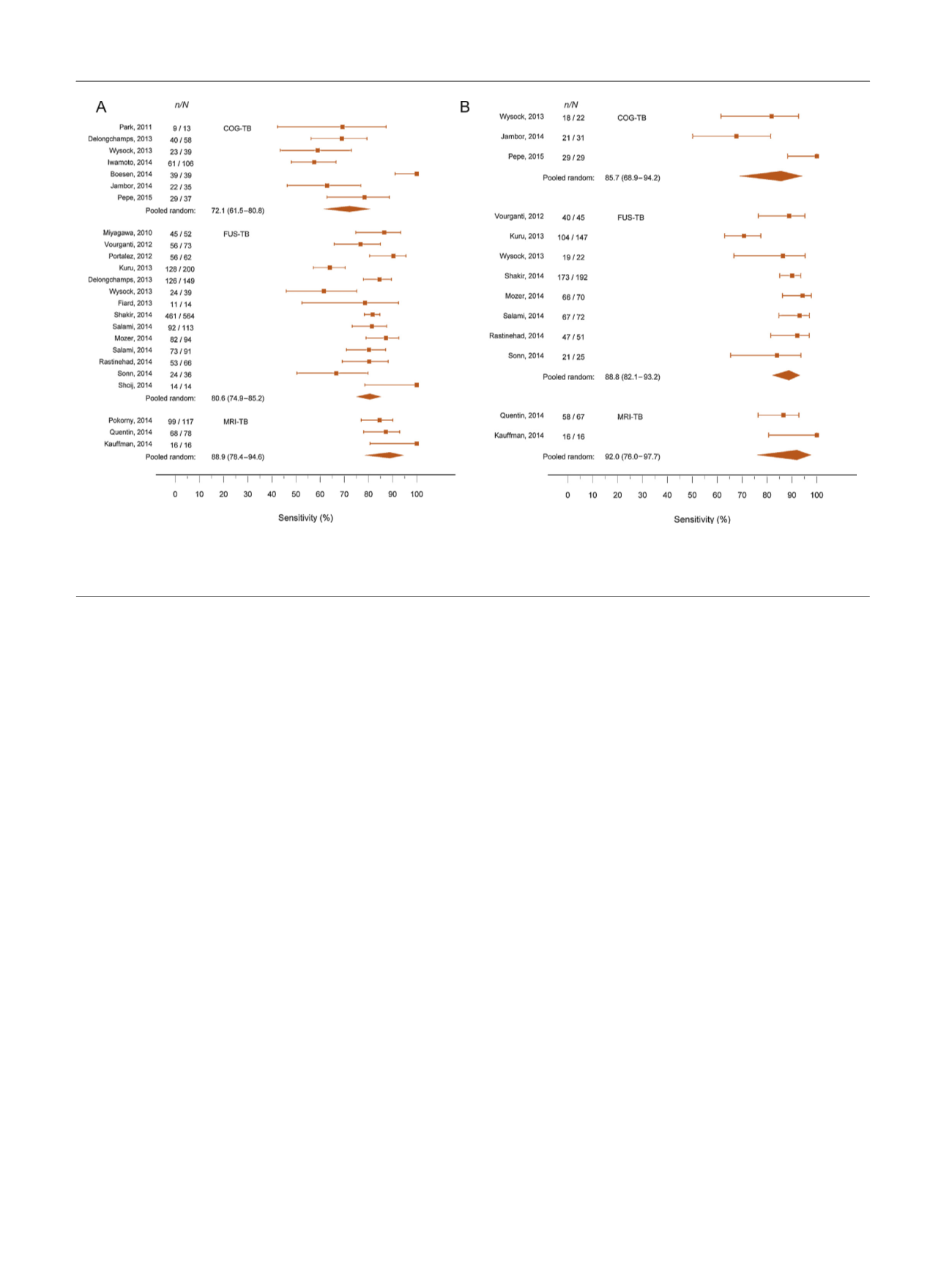
[(Fig._3)TD$FIG]
Fig. 3 – (A) Forest plots of pooled sensitivity of cognitive registration transrectal ultrasound-targeted biopsy (COG-TB), magnetic resonance imagimg-
TRUS fusion TB (FUS-TB), and MRI-TB for all prostate cancer; (B) forest plots of pooled sensitivity of COG-TB, FUS-TB, and MRI-TB for clinically
significant prostate cancer.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 5 1 7 – 5 3 1
526
















