
Patients undergoing PN were younger (WMD 2.3 yr,
95% CI –3.5 to –1.1;
p
<
0.001) and had smaller masses
(WMD –0.65 cm, 95% CI –0.81. to –0.49;
p
<
0.001), whereas
there was no difference for baseline renal function, as
determined by baseline eGFR (WMD –0.50 ml/min, 95% CI –
3.2 to 2.2;
p
= 0.72). Similarly, there was no difference in the
proportion of patients with baseline CKD (RR 1.5, 95% CI
0.94–2.4;
p
= 0.09). There was also no difference in length of
follow-up between PN and RN patients (
p
= 0.27).
There was no significant difference in operative time
(WMD –10.9 min, 95% CI –17.8 to 39.6;
p
= 0.46), but there
was lower estimated blood loss for RN (WMD –102.6 ml,
95% CI 45.7, 159.5;
p
<
0.001). The likelihood of postopera-
tive complications was higher for PN (OR 1.74, 95% CI 1.34–
2.2;
p
<
0.001;
Fig. 2). Length of hospital stay was similar for
the two procedures (WMD –0.1 d, 95% CI –1.07 to 0.88;
p
= 0.84). On pathology there was a higher rate of malignant
histology for the RN group (RR 0.97, 95% CI 0.95–1.00;
p
= 0.02).
PN was associated with better postoperative renal
function, as shown by higher postoperative eGFR (WMD
12.4 ml/min, 95% CI 9.8–14.9;
p
<
0.001), lower likelihood
of onset of postoperative CKD (RR 0.36, 95% CI 0.52–0.76;
p
<
0.001), and lower decline in eGFR (WMD –8.6 ml/min,
95% CI –12.6 to –4.7;
p
<
0.001;
Fig. 3 ).
The likelihood of tumor recurrence was lower for PN (OR
0.6, 95% CI 0.46–0.79;
p
<
0.001), as was the likelihood of
cancer-specific mortality (OR 0.58, 95% CI 0.41–0.81;
p
= 0.001) and all-cause mortality (OR 0.67, 95% CI 0.51–
0.88;
p
= 0.005;
Fig. 4 ).
3.2.
PN versus RN for cT2 only tumors
Four studies compared PN (
n
= 212) to RN (
n
= 1792) in the
specific case of T2 (
>
7 cm) tumors
( Table 1)
[13,24,41– 43]. There was no difference in terms of age (WMD –2.6 yr,
95% CI –6.3 to 1.1;
p
= 0.17), but tumor size was smaller for
PN (WMD –1.8 cm, 95% CI –3.3 to –0.3;
p
= 0.02).
With regard to surgical outcomes, higher estimated
blood loss was found for PN (WMD 107.6 ml, 95% CI 84.4–
130.7;
p
<
0.001), as well as a higher likelihood of
complications (RR 2.0, 95% CI 1.5–2.7;
p
<
0.001;
Fig. 5 ).
Length of hospital stay was longer for PN, but the difference
did not reach statistical significance (WMD 0.7 d, 95% CI –
0.1 to 1.5;
p
= 0.11).
The recurrence rate was lower for the PN group (RR 0.61,
95% CI 0.44–0.86;
p
= 0.004), as was cancer-specific
mortality (RR 0.65, 95% CI 0.44–0.97;
p
= 0.03), but there
was no significant difference in all-cause mortality (RR 0.76,
95% CI 0.56–1.03;
p
= 0.07;
Fig. 5).
3.3.
Interpretation of the data
We report the first meta-analysis of studies comparing PN
to RN for larger (T1b and T2) renal masses, for which the role
of nephron-sparing surgery is still debated. The present
analysis of a large pooled sample (
>
10 000 cases) can
contribute to the ongoing debate, ultimately paving the way
for further research on this topic, and provides key
information for contemporary evidence-based patient
counseling. Overall, we found that PN in these cases is a
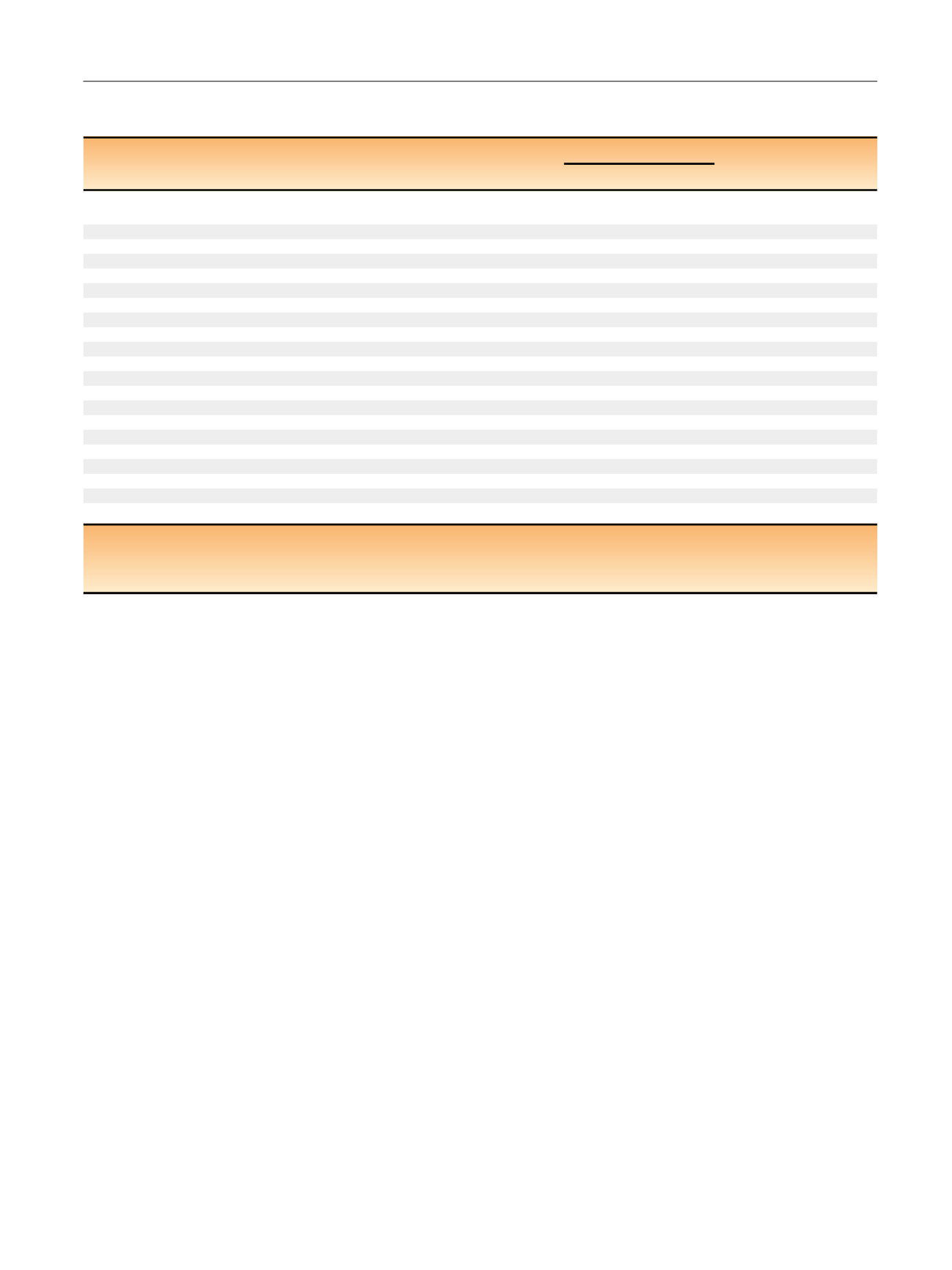
Table 1 – Studies included in the meta-analysis for assessment of outcomes for partial nephrectomy (PN) versus radical nephrectomy (RN)
for cT1b and higher renal tumors
Reference
Study period Study design
Study origin
T stage
PN/RN
Surgical
SQ LE
Cases (
n
)
Mean FU (mo)
technique
Patard
[25]1984–2001
RTP, MI
France, Netherlands,
Italy, USA
T1b–2
379/1075
50.7/66.6
Open
7 III
Dash
[26]1998–2004
RTP, PS, MI
USA
T1b–2
45/151
21^
Open
7 III
Mitchell
[27]1988–2004
RTP, SC
USA
T1b–2
33/66
34/48.5
aOpen
7 III
Simmons
[28]2001–2005
RTP, SC
USA
T1b–2
35/75
50/55
Lap
7 III
Antonelli
[29]1983–2007
RTP, SC
Italy
T1b–2
52/277
59.2/78.8
Open
7 III
Thompson
[30]1989–2006
RTP, MI
USA
T1b–2
286/873
40.8/63.6
aOpen/Lap
7 III
Weight
[31]1999–2006
RTP, SC
USA
T1b–2
524/480
50/46
Open/Lap
7 III
Deklaj
[32]2002–2008
RTP, SC
USA
T1b–2
33/60
15/21
Lap
7 III
Kim
[33]1995–2004
RTP, SC
Korea
T1b–2
18/52
78.2/66.5
Open
7 III
Weight
[34]1999–2006
RTP, SC
USA
T1b–2
212/298
49/41
aOpen/Lap
7 III
Antonelli
[35]1995–2007
RTP, MI
Italy
T1b–2
198/1426
47
aOpen/Lap
7 III
Roos
[22,23] b1988–2007
RTP, SC
Germany
T1b–2
188/641
83.1/97.5
Open
7 III
Iizuka
[36]1979–2011
RTP, SC
Japan
T1b–2
67/195
31.3/52.7
Open
7 III
Brewer
[37]2004–2010
RTP, SC
USA
T1b–2
45/180
NS
Lap/robotic
7 III
Milonas
[38]1998–2009
RTP, SC
Lithuania
T1b–2
34/317
74.7/76.8
Open
7 III
Pignot
[39]1984–2001
RTP, MI
France, Italy, USA
T1b–2
123/185
39.5/46.9
NS
7 III
Jang
[40]1999–2011
RTP, PM, MI
Korea
T1b–2
100/477
48.1/42.6
Open
7 III
Margulis
[41]1990–2006
RTP, SC
USA
T2 only 34/567
62.1/43.4
NS
8 III
Jeldres
[42]1984–2001
RTP, MI
Canada, France
T2 only 29/896
57.6/55.2
NS
8 III
Brea
u [43]1970–2008
RTP, PM, SC USA
T2 only 69/207
38.4
aNS
8 IIa
Kopp
[14,24] b2002–2012
RTP, MI
USA
T2 only 80/122
41.5
aOpen/Lap
8 III
FU = follow-up; SQ = study quality according to the Newcastle-Ottawa scale; LE = level of evidence according to the Oxford Centre for Evidence-based Medicine;
RTP = retrospective; MI = multi-institutional; SC = single center; PS = propensity score; PM = pair matched; NS = not specified; Lap = laparoscopic.
a
Median.
b
These groups reported two separate analyses for the same data set (see the text).
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 6 0 6 – 6 1 7
609
















