
153 (68.3%) in patients with nonorthotopic bladder sub-
stitutes. From a clinical perspective, this finding is likely a
selection bias as patients with advanced tumor stage,
prostatic urethral disease, or extensive CIS were more likely
to receive incontinent diversions. However, one may also
hypothesize that connecting urothelial and intestinal tissue
induces immune reactions resulting in an enhancement of
the local immune response to carcinogenic antigens. A
recent study immunohistochemically investigated urethral
tissues obtained from seven neobladder patients and nine
healthy controls
[19]. In neobladder patients, there was a
nonsignificant trend towards a higher relative fraction of B-
cells, especially CD138 positive plasma cells, and a lower
relative fraction of T-cells
[19]. Yet, whether this immuno-
logical finding may be causative for the apparently lower
risk of secondary urethral tumors in neobladder patients is
unclear. This study lacked a comparative group of patients
undergoing cystectomy with ileal conduit. As studies
evaluating risk factors for secondary upper tract malignan-
cies did not find OBS to be associated with a reduced risk of
metachronous UTUC
[6], connecting urethral and intestinal
tissue may not per se induce immunological changes.
Instead, the constant flow of neobladder urine through the
retained urethra may lead to immuno-inductive processes.
Another possible explanation is the potential for earlier
diagnosis of recurrence in patients with orthotopic diver-
sion due to their voiding through the urethra. It is more
likely that conduit patients who develop urethral recur-
rence may also present with advanced disease due to a large
local recurrence. These considerations suggest that follow-
up for patients with ileal conduit should include urethral
inspection or cytology obtained with brushing.
3.2.
Accuracy and prognostic significance of frozen section
analysis of urothelial margins at RC
3.2.1.
Ureteral frozen section analysis
In contemporary RC series, the rate of positive ureteral
margins on permanent sections ranges between 6.8% and
14.0%
( Table 3)
[20–23] .Tumor multifocality
[23] ,a positive
FSA of the distal ureter
[21,23], male sex
[21] ,and the
presence of bladder CIS
[22,24]were found to indepen-
dently predict malignancy at the distal ureteral margin on
permanent section. For ureteral FSA, the majority of studies
have reported sensitivity and specificity rates around
75–80% and 95–99%, respectively
[20,22,23,25]. A large
study on 2047 patients treated with RC over a time period of
40 yr investigated the accuracy of intraoperative FSA of the
ureteral margins. The sensitivity of FSA for correctly
predicting the final ureteral margin status was only 59%
and showed only a moderate increase to 69% for CIS
[8]. The
rate of secondary UTUC was noticeably low at 1.4% (
N
= 28)
and no recurrences were observed at the ureteroileal
anastomosis. A positive FSA was associated with meta-
chronous UTUC only in univariable analysis. In addition,
authors reported that 15 of the 28 patients (54%) with
subsequent UTUC had negative results for FSA of the
ureteral margins. While these data question the utility of
routine FSA for the intraoperative assessment of the distal
ureters, some consideration needs to be given to the
interpretation of these results. Although the sample size is
large, it covers a period of almost 40 yr which may have
implications on histopathologic assessment during the
study period. The reported sensitivity for the detection of
malignancy at the margin was considerably less than in
other series and the rate of metachronous UTUC after a
median follow-up of more than 12 yr was exceptionally low.
Malignant ureteral margins on permanent section show
CIS or severe dysplasia in more than 75% of the cases
[25]. Various series have demonstrated that the presence of
CIS at the ureteral margin on permanent section after RC
carries an increased risk of metachronous UTUC
[22,23] .Moreover, prior studies have suggested that patients with
SUTs at the ureteroileal anastomosis have a higher risk for
cancer-specific death compared with patients with proximal
tumors
[26,27]. Thus, one may hypothesize that converting a
positive margin into a negative one by means of reresec-
tion(s) impacts favorably on prognosis. However, the
presence of
skip
lesions, or pagetoid spread, particularly
for CIS, limits the therapeutic value of obtaining a negative
FSA for preventing metachronous UTUC. A recent study
investigated the presence of
skip
lesions in patients who had
at least two resections of the same ureter at RC
[25] .Skip
lesions were found in 5% of the patients, with CIS being the
most prevalent histological malignant entity.
Skip
lesions
were associated with lymphovascular invasion and non-
muscle invasive disease at RC and were also associated with
a lower overall survival. These findings suggest that
skip
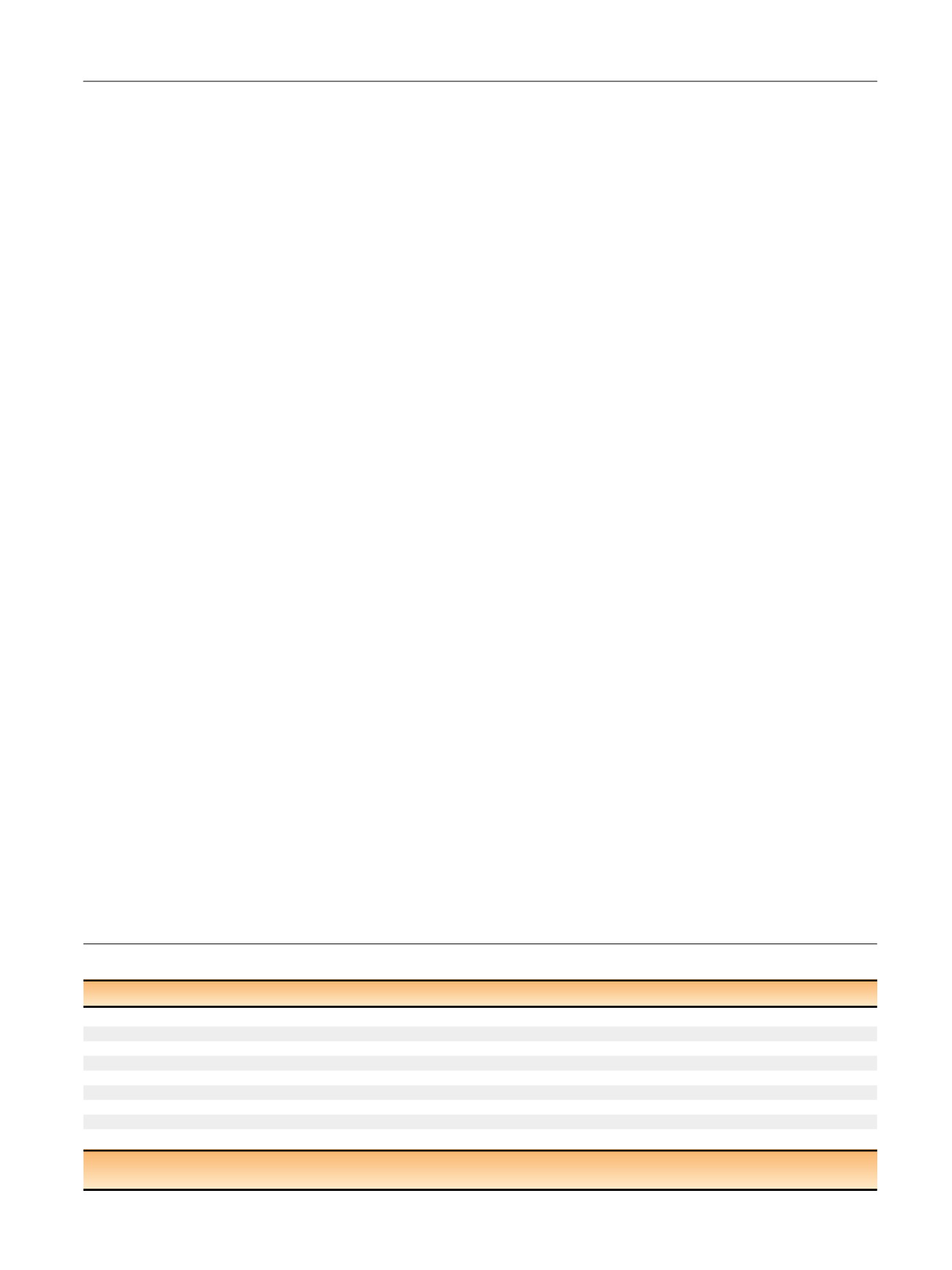
Table 3 – Assessment of urothelial malignancy at radical cystectomy with different methods
Study
Site
Method
N
total
N
(malig.)
Sensitivity (%)
Specificity (%)
PPV (%)
NPV (%)
Accuracy
Satkunasivam [
[70_TD$DIFF]
8]
Ureter
FSA
2047
178 (8.6)
59
93
n.r.
n.r.
n.r.
Kim [
[71_TD$DIFF]
20]
Ureter
FSA
402
46 (11.2)
75
96
n.r.
n.r.
95
Osman [
[72_TD$DIFF]
21]
Ureter
FSA
100
14 (14.0)
45
98
81
91
n.r.
Raj [
[73_TD$DIFF]
22]
Ureter
FSA
1330
171 (12.9)
75
99
n.r.
n.r.
n.r.
Gakis [
[74_TD$DIFF]
23]
Ureter
FSA
218
15 (6.8)
74
100
94
99
98
Osman [
[75_TD$DIFF]
34]
Urethra
FSA
100
6 (6.0)
33
99
83
89
89
von Rundstedt [
[76_TD$DIFF]
39]
Urethra
TUPBx
272
101 (37.1)
71
100
100
86
89
Gaya [
[77_TD$DIFF]
40]
Urethra
TUPBx
234
81 (34.6)
81
82
62
92
n.r.
Ichihara [
[78_TD$DIFF]
63]
Urethra
TUPBx
101
25 (24.8)
86
91
72
96
n.r.
FSA = frozen section analysis; malig. = malignant;
N
= number of patients; NPV = negative predictive value; n.r. not reported; PPV = positive predictive value;
TUPBx = transurethral prostatic urethral biopsy.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 5 4 5 – 5 5 7
551
















