
and contemporary RN cohorts, we found statistically
significant differences in age, the presence of symptoms
at diagnosis, eGFR, ECOG status, CCI, BMI, pT and pN
classifications, tumor size, grade, and necrosis. Notably,
SSIGN scores were significantly higher in the contemporary
RN compared with the original cohort (median score 5 vs 4;
p
<
0.001).
When the contemporary RN and PN cohorts were
compared, we found statistically significant differences in
age, the presence of symptoms at diagnosis, eGFR, ECOG,
CCI, BMI, the pT, pN, andM classifications, tumor size, grade,
necrosis, and sarcomatoid differentiation. As anticipated,
SSIGN scores were significantly higher in the contemporary
RN compared with the PN cohort (median score 5 vs 0;
p
<
0.001).
3.2.
Survival assessment by cohort
At last follow-up, 1571 patients in the original RN cohort
had died including 802 who died from RCC. The median
duration of follow-up for the 224 patients alive at last
follow-up was 20.1 yr (IQR: 16.5–25.2). Each increase in
SSIGN score was associated with an HR of 1.41 (95% CI,
1.38–1.44;
p
<
0.001) for death from RCC, with a bootstrap-
corrected C-index of 0.82. After adjusting for the competing
risk of non-RCC death, higher SSIGN scores remained
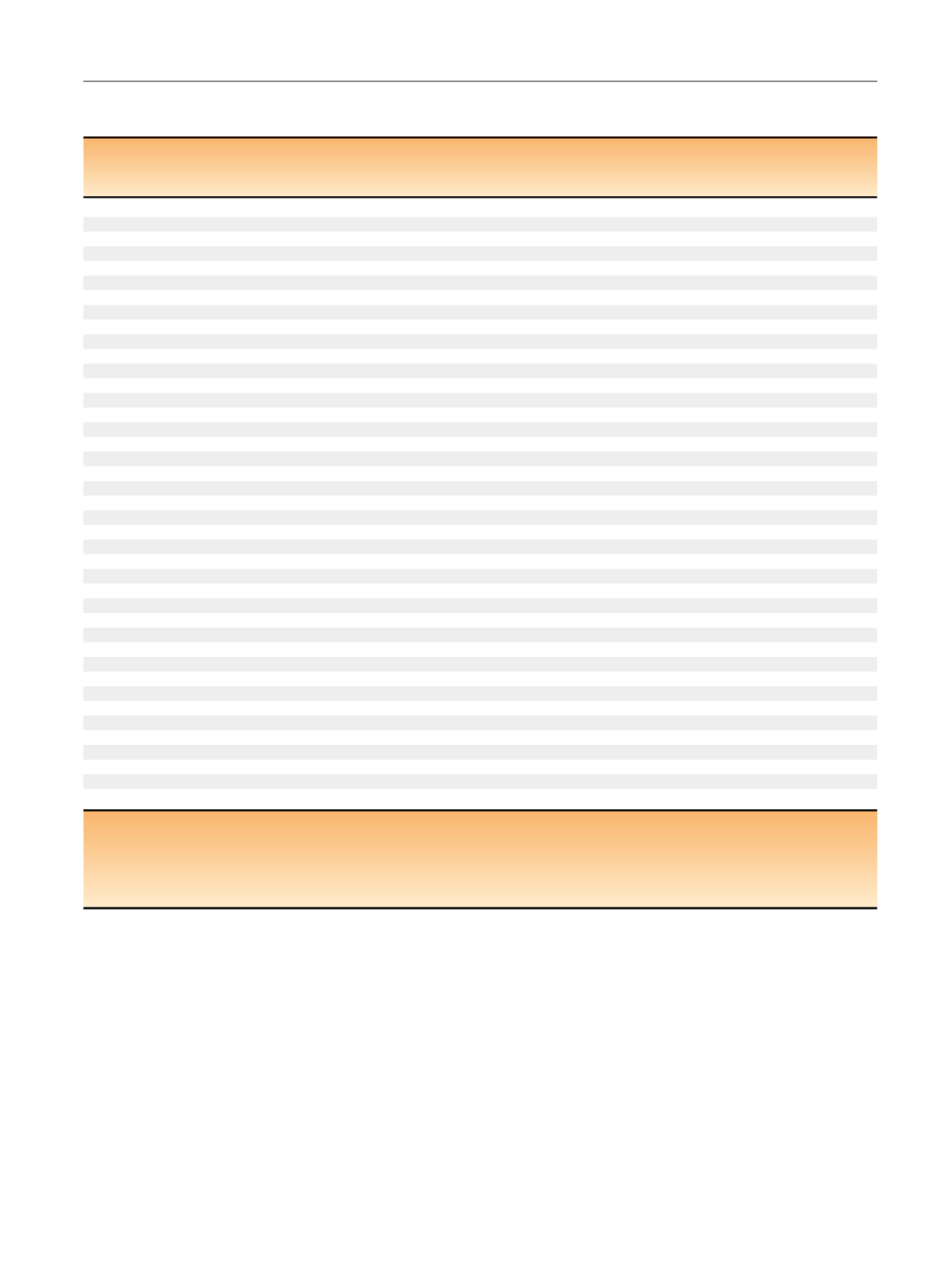
Table 1 – Clinicopathologic features of patients in the original radical nephrectomy (RN), contemporary RN, and contemporary partial
nephrectomy (PN) cohort
s *Original
RN
n
= 1795
p
value
y
Contemporary
RN
n
= 1038
p
value
z
Contemporary
PN
n
= 767
Feature
Median (IQR) or
n
(%)
Age at surgery, yr
63 (54–70)
0.031
64 (55–72)
<
0.001
60 (51–69)
Male gender
1150 (64)
0.21
689 (66)
0.22
488 (64)
ECOG performance status (
n
= 1365, 1037, 765)
<
0.001
<
0.001
0
1184 (87)
820 (79)
682 (89)
1
141 (10)
148 (14)
56 (7)
2
40 (3)
69 (7)
27 (4)
Charlson Comorbidity Index (
n
= 1362, 1038, 765
) **1 (0–2)
<
0.001
1 (0–3)
<
0.001
1 (0–2)
BMI (
n
= 1244, 980, 735)
27 (24–30)
<
0.001
29 (25–33)
0.002
30 (26–34)
eGFR (
n
= 1777, 1022, 753)
65 (53–78)
<
0.001
62 (51–74)
<
0.001
72 (58–86)
Smoking history (
n
= 1744, 1026, 754)
0.43
0.90
Never
734 (42)
416 (41)
308 (41)
Current/former
1010 (58)
610 (59)
446 (59)
Symptoms (
n
= 1786, 1037, 766)
1292 (72)
<
0.001
633 (61)
<
0.001
208 (27)
Constitutional symptoms (
n
= 1786, 1037, 766)
600 (34)
<
0.001
262 (25)
<
0.001
49 (6)
pT stage
<
0.001
<
0.001
pT1a
356 (20)
136 (13)
550 (72)
pT1b
430 (24)
209 (20)
175 (23)
pT2a
248 (14)
123 (12)
18 (2)
pT2b
114 (6)
56 (5)
3 (
<
1)
pT3a
480 (27)
363 (35)
21 (3)
pT3b
136 (8)
103 (10)
0
pT3c
12 (1)
16 (2)
0
pT4
19 (1)
32 (3)
0
pN stage
<
0.001
<
0.001
pNX
668 (37)
552 (53)
743 (97)
pN0
1028 (57)
379 (37)
24 (3)
pN1
99 (6)
107 (10)
0
M stage
0.12
<
0.001
M0
1510 (84)
850 (82)
762 (99)
M1
285 (16)
188 (18)
5 (1)
Tumor size
<
0.001
<
0.001
<
5 cm
496 (28)
217 (21)
646 (84)
5 cm
1299 (72)
821 (79)
121 (16)
Grade
<
0.001
<
0.001
1
182 (10)
44 (4)
114 (15)
2
777 (43)
278 (27)
448 (58)
3
676 (38)
525 (51)
193 (25)
4
160 (9)
191 (18)
12 (2)
Coagulative tumor necrosis
553 (31)
<
0.001
439 (42)
<
0.001
42 (5)
Sarcomatoid differentiation
100 (6)
0.93
57 (5)
<
0.001
2 (
<
1)
SSIGN score
4 (2–7)
<
0.001
5 (3–9)
<
0.001
0 (0–1)
BMI = body mass index; ECOG = Eastern Cooperative Oncology Group; eGFR = estimated glomerular filtration rate; PN = partial nephrectomy; RN = radical
nephrectomy; SSIGN = stage, size, grade, and necrosis.
*
Sample sizes for features with missing data for the three cohorts are indicated in parentheses.
y
The
p
value represents the difference between the original RN and contemporary RN cohorts.
z
The
p
value represents the difference between the contemporary RN and PN cohorts.
**
Mean Charlson scores for the three groups were 1.8, 2.2, and 1.2, respectively.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 6 6 5 – 6 7 3
667
















