
soft tissue lesion using the Response Evaluation Criteria
in Solid Tumours
[8,25]Symptomatic progression alone must be questioned and
subject to further investigation; it is not sufficient for
diagnosing CRPC.
Post-treatment PSA surveillance has resulted in earlier
detection of progression. Although approximately one-third
of men with rising PSA will develop bone metastases within
2 yr
[69], no available studies suggest a benefit for
immediate treatment. In men with CRPC and no detectable
clinical metastases, baseline PSA level, PSA velocity, and PSA
DT have been associated with time to first bone metastasis,
bone metastasis-free survival, and OS
[69,70]. These factors
may be used when deciding which patients should be
evaluated for metastatic disease. A consensus statement by
the Prostate Cancer Radiographic Assessments for Detection
of Advanced Recurrence (RADAR) group
[71]suggested that
a bone scan be performed when PSA reached 2 ng/ml and
that if this was negative, it should be repeated when PSA
reached 5 ng/ml and again after every doubling of the PSA
based on PSA testing every 3 mo for asymptomatic men.
Symptomatic patients should undergo relevant investiga-
tion regardless of PSA level
( Table 5).
Two trials have shown a marginal survival benefit for
patients with metastatic CRPC (mCRPC) remaining on LHRH
analogues during second- and third-line therapies
[72,73] .In
addition, all subsequent treatments have been studied in
men with ongoing androgen suppression; therefore, it
should be continued indefinitely in these patients.
4.2.
First-line treatment in metastatic castration-resistant
prostate cancer
Abiraterone was evaluated in 1088 chemonaı¨ve mCRPC
patients in the phase 3 trial COU-AA-302. Patients were
randomised to abiraterone acetate or placebo, both com-
bined with prednisone
[74] .The main stratification factors
were ECOG performance status 0 or 1 and asymptomatic or
mildly symptomatic disease. OS and radiographic PFS (rPFS)
were the co–primary end points. After a median follow-up of
22.2 mo, there was significant improvement of rPFS
(median: 16.5 vs 8.2 mo; HR: 0.52;
p
<
0.001), and the
trial was unblinded. At the final analysis, with a median
follow-up of 49.2 mo, the OS end point was significantly
positive (34.7 vs 30.3 mo; HR: 0.81; 95% CI, 0.70–0.93;
p
= 0.0033)
[75] .AEs related to mineralocorticoid excess and
liver function abnormalities were more frequent with
abiraterone but were mostly grades 1–2.
A randomised phase 3 trial (PREVAIL)
[76]included a
similar patient population and compared enzalutamide and
placebo. Men with visceral metastases were accepted,
although the numbers were small. Corticosteroids were
allowed but were not mandatory. PREVAIL was conducted in
a chemonaı¨ve mCRPC population of 1717 men and showed
significant improvement in both co–primary end points of
rPFS (HR: 0.186; 95% CI, 0.15–0.23;
p
<
0.0001) and OS (HR:
0.706; 95% CI, 0.6–0.84;
p
<
0.001). The most common
clinically relevant AEs were fatigue and hypertension.
In 2010, a phase 3 trial of sipuleucel-T showed a survival
benefit in 512 asymptomatic or minimally symptomatic
mCRPC patients
[77]. After a median follow-up of 34 mo,
median survival was 25.8 mo in the sipuleucel-T group
compared with 21.7 mo in the placebo group, leading to a
significant HR of 0.78 (
p
= 0.03). No PSA decline was
observed, and PFS was equivalent in both arms. Overall
tolerance was very good, with more cytokine-related grade
1–2 AEs in the sipuleucel-T group but the same amount of
grade 3–4 AEs in both arms. Sipuleucel-T is not available in
Europe.
A significant improvement in median survival of 2.0–2.9
mo occurred with docetaxel-based chemotherapy com-
pared with mitoxantrone plus prednisone therapy
[78]. The
standard first-line chemotherapy is docetaxel 75 mg/m
2
in
three weekly doses combined with prednisone 5 mg twice a
day up to 10 cycles. Prednisone can be omitted if there are
contraindications or no major symptoms. Several poor
prognostic factors have been described before docetaxel
treatment: PSA
>
114 ng/ml, PSA DT
<
55 d, or the presence
of visceral metastases
[79]. A better risk group definition
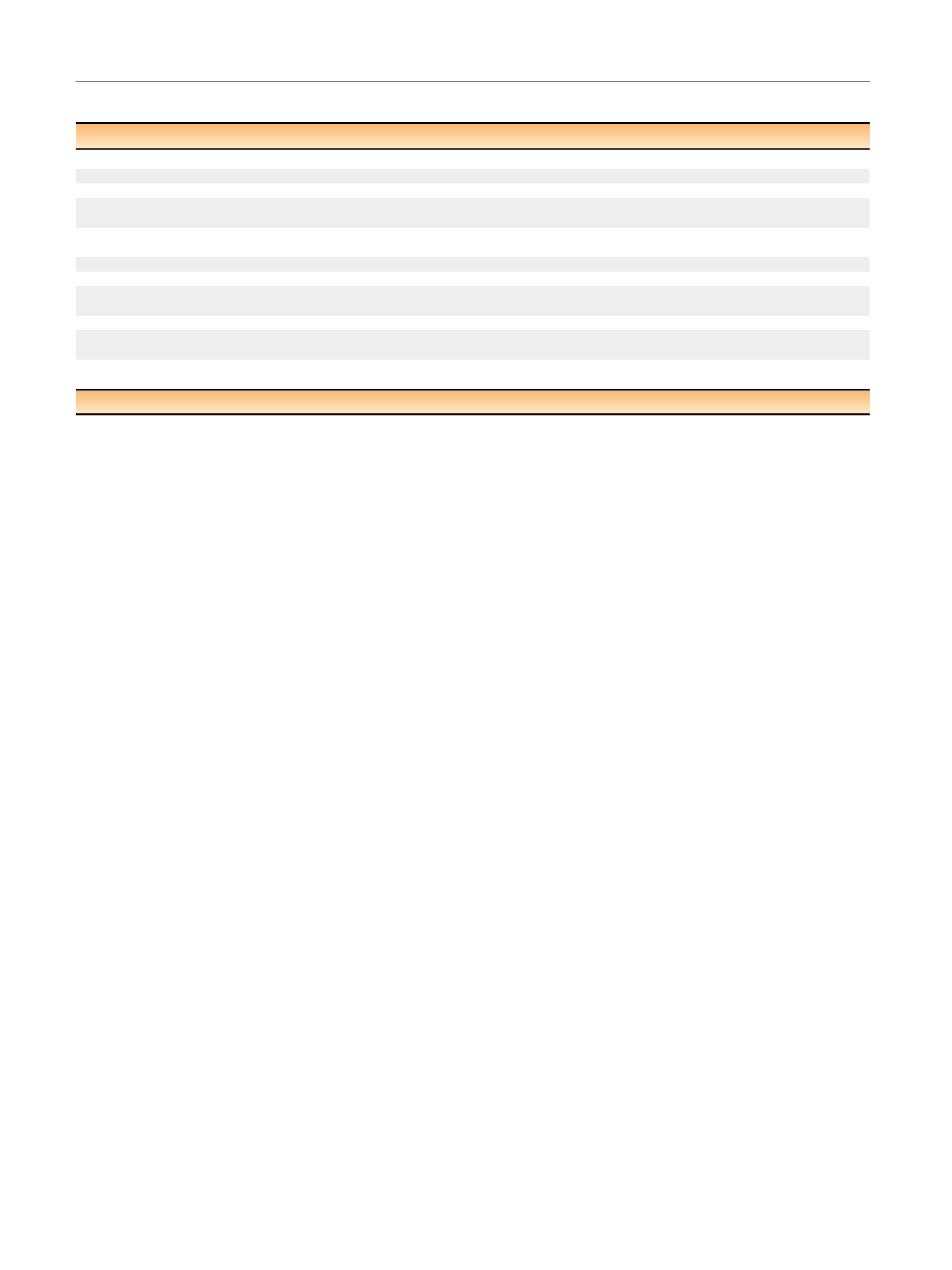
Table 5 – Guidelines for management of castration-resistant prostate cancer
Recommendation
LE
GR
Ensure that testosterone levels are confirmed to be
<
50 ng/ml before diagnosing CRPC.
4
A
Do not treat patients for nonmetastatic CRPC outside of a clinical trial.
3
A
Counsel, manage, and treat patients with mCRPC in a multidisciplinary team.
3
A
In men treated with maximal androgen blockade, stop antiandrogen therapy once PSA progression is documented.
Comment: At 4–6
wk after discontinuation of flutamide or bicalutamide, an eventual antiandrogen withdrawal effect will be apparent.
2a
A
Treat patients with mCRPC with life-prolonging agents. Base the choice of first-line treatment on the performance status, symptoms,
comorbidities, and extent of disease (alphabetical order: abiraterone, cabazitaxel docetaxel, enzalutamide, Ra 223, sipuleucel-T).
1b
A
Offer patients with mCRPC who are candidates for cytotoxic therapy, docetaxel with 75 mg/m
2
every 3 wk.
1a
A
Base second-line treatment decisions of mCRPC on pretreatment performance status, comorbidities, and extent of disease.
B
Offer bone-protective agents to patients with skeletal metastases to prevent osseous complications; however, the benefits must be
balanced against the toxicity of these agents, and jaw necrosis in particular must be avoided.
1a
B
Offer calcium and vitamin D supplementation when prescribing either denosumab or bisphosphonates.
1b
A
Treat painful bone metastases early on with palliative measures such as external beam radiotherapy, radionuclides, and adequate use
of analgesics.
1a
B
In patients with spinal cord compression, start immediate high-dose corticosteroids and assess for spinal surgery followed by irradiation.
Offer radiation therapy alone if surgery is not appropriate.
1b
A
CRPC = castration-resistant prostate cancer; GR = grade of recommendation; LE = level of evidence; mCRPC = metastatic castration-resistant prostate cancer.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 6 3 0 – 6 4 2
636
















