
patients with rising PSA and/or clinical progression, serum
testosterone must be evaluated in all cases to confirm a
castrate-resistant state.
During long-term therapy, ADT reduces bone mineral
density (BMD) and increases the risk of fractures
[65] .In the
absence of associated risk factors, it is recommended that
BMD and serum vitamin D and calcium levels should be
measured every 2 yr
[66]. Treatment should be individual-
ised; however, for men with a BMD T-score lower than 2.5
and one risk factor or more or with hip and vertebral
fractures, use of bisphosphonates should be discussed.
Specialists should also screen patients for the development
of metabolic sequelae associatedwith ADT such as alterations
in lipid profiles and decreased insulin sensitivity
[67]. Al-
though little is known about the optimal strategy to mitigate
the adverse metabolic effects, the Guidelines Panel recom-
mends treatment strategies to reduce the risk of diabetes and
cardiovascular disease
[68] .Patients should be given advice
on modifying their lifestyle (eg, diet, exercise, smoking
cessation) and should be treated for any existing conditions,
such as diabetes, hyperlipidaemia, and/or hypertension.
Furthermore, the risk–benefit ratio of ADT must be consid-
ered for patients with a higher risk of cardiovascular
complications, especially if it is possible to delay starting
ADT.
4.
Castration-resistant prostate cancer
( Table 4 )4.1.
Definition
CRPC is defined as castrate serum testosterone
<
50 ng/dl or
1.7 nmol/l plus one of the following types of progression:
Biochemical progression: Three consecutive rises in PSA
1 wk apart, resulting in two 50% increases over the nadir,
and PSA
>
2 ng/ml
Radiologic progression: The appearance of new lesions:
either two or more new bone lesions on bone scan or a
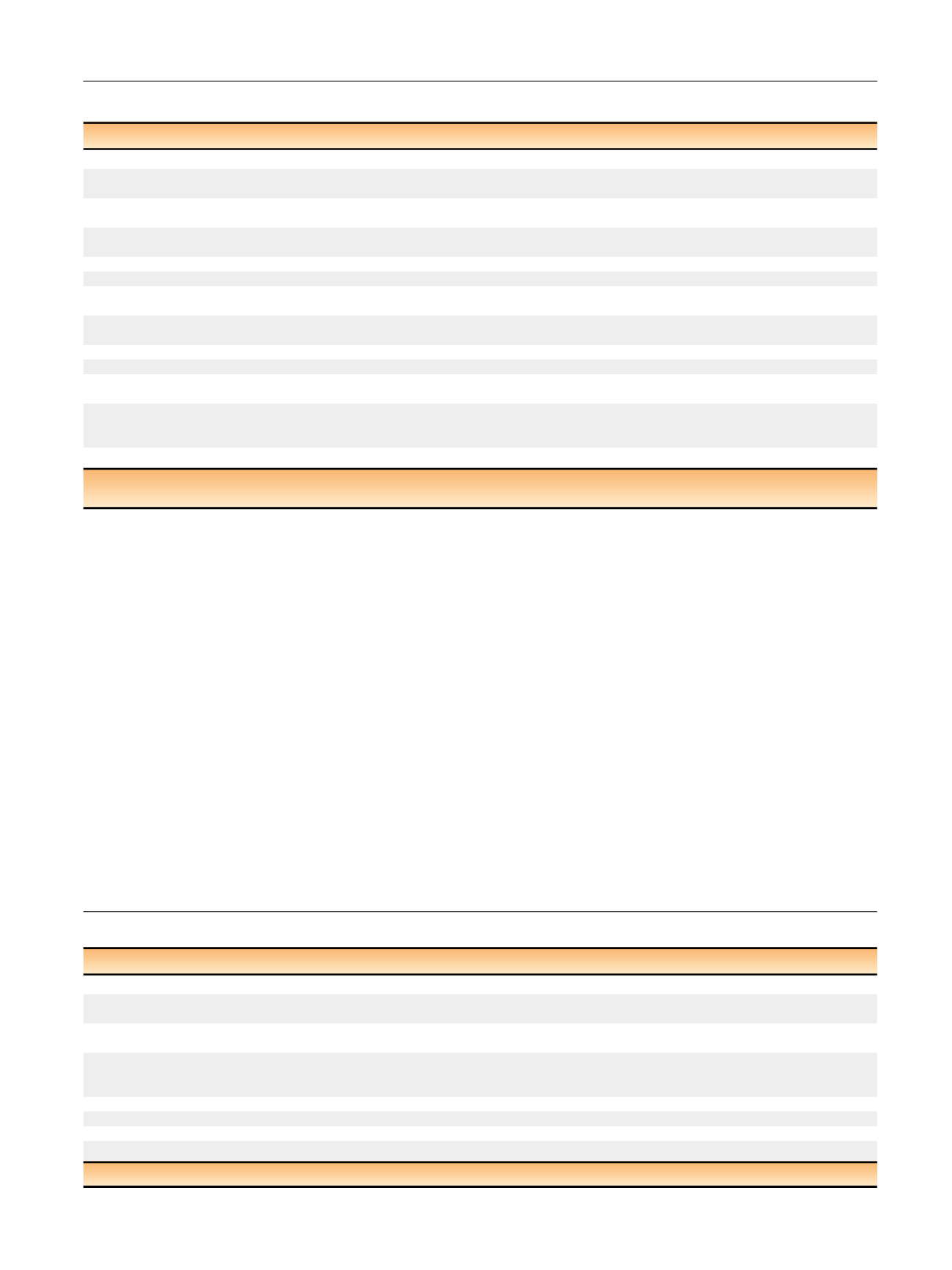
Table 3 – Guidelines for hormonal treatment of metastatic prostate cancer
Recommendation
LE GR
In newly diagnosed M1 patients, offer castration combined with docetaxel, provided patients are fit enough to receive chemotherapy.
1a
A
In M1 symptomatic patients, offer immediate castration to palliate symptoms and reduce the risk of potentially catastrophic sequelae of
advanced disease (spinal cord compression, pathologic fractures, ureteral obstruction, extraskeletal metastasis).
1b A
In M1 asymptomatic patients, offer immediate castration to defer progression to a symptomatic stage and prevent serious disease
progression-related complications.
1b A
In M1 asymptomatic patients, discuss deferred castration with well-informed patients because it lowers the treatment side effects, provided
the patient is closely monitored.
2b B
Anti-androgens
Offer LHRH antagonists, especially in patients with an impending spinal cord compression or bladder outlet obstruction.
2
B
In M1 patients treated with an LHRH agonist, offer short-term administration of antiandrogens to reduce the risk of the ‘‘flare-up’’
phenomenon.
2a
A
Start antiandrogens used for flare-up prevention on the same day that an LHRH analogue is started or for up to 7 d before the first LHRH
analogue injection if patient has symptoms. Treat for 4 wk.
3
A
Do not offer antiandrogen monotherapy in M1 patients.
1a
A
Intermittent treatment
Population
In asymptomatic M1 patients, offer intermittent treatment to highly motivated men with a major PSA
response after the induction period.
1b B
Threshold to start and stop ADT
In M1 patients, follow the schedules used in published clinical trials on timing of intermittent
treatment. Stop treatment when the PSA level is
<
4 ng/ml after 6–7 mo of treatment.
Resume treatment when the PSA level is
>
10–20 ng/ml (or to the initial level if
<
20 ng/ml).
1b B
Drugs
In M1 patients, offer combined treatment with LHRH agonists and NSAA.
1b A
ADT = androgen deprivation therapy; GR = grade of recommendation; LE = level of evidence; LHRH = luteinising hormone-releasing hormone;
NSAA = nonsteroidal antiandrogen; PSA = prostate-specific antigen.
Table 4 – Guidelines for follow-up during hormonal treatment
Recommendation
GR
Evaluate patients at 3–6 mo after the initiation of treatment.
A
As a minimum, tests should include serum PSA measurement, physical examination, serum testosterone, and careful evaluation of symptoms to
assess the treatment response and side effects.
A
In patients undergoing intermittent androgen deprivation, monitor PSA and testosterone at fixed intervals during the treatment pause
(at 3-mo intervals).
A
In patients with stage M1 disease with good treatment response, schedule follow-up every 3–6 mo. As a minimum requirement, include a
disease-specific history, physical examination, serum PSA, haemoglobin, and serum creatinine and alkaline phosphatase measurements in the
diagnostic work-up. The testosterone level should be checked, especially during the first year.
A
Counsel patients (especially with M1b status) about the clinical signs suggestive of spinal cord compression.
A
When disease progression occurs or if the patient does not respond to treatment, adapt/individualise follow-up.
A
In patients with suspected progression, assess the testosterone level. By definition, CRPC requires a testosterone level
<
50 ng/ml (
<
1.7 nmol/l).
B
Do not offer routine imaging to otherwise stable patients.
B
CRPC = castration-resistant prostate cancer; GR = grade of recommendation; LE = level of evidence; PSA = prostate-specific antigen.
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 6 3 0 – 6 4 2
635
















