
10-yr follow-up. Seven of these 23 patients (30%) were cases
of wet OAB. During the last visit, only one patient reported
persistent voiding difficulties, but this woman did not need
any treatment. No patient required tape release or resection
during these 10 yr. No significant POP or vaginal, bladder, or
urethral erosion was registered in our study population.
One patient noted persistent mild groin pain at 10-yr
follow-up with a visual analog scale score of 2 of 10, not
requiring analgesic treatment. Four of 92 sexually active
patients (4.3%) noted dyspareunia at 10 yr, when asked
whether they feel pain during intercourse. In these cases,
we prescribed a local estrogenic treatment.
4.
Discussion
This study reports the combination of subjective and
objective outcomes of TVT-O at 10-yr follow-up. We found
that TVT-O is a highly effective and safe procedure. The
10-yr objective and subjective cure rates were both
95%, showing that TVT-O has long-lasting effectiveness.
Use of the MUS is widely considered the gold-standard
procedure for the surgical treatment of female SUI. A recent
systematic review and meta-analysis showed that retro-
pubic MUS and transobturator MUS have similar objective
cure rates in the long- and medium-term, but transobtura-
tor tapes (TOTs) have a lower subjective cure rate than TVT
[26]. Although the long-lasting benefits of the retropubic
route were adequately evaluated
[5,6], data are lacking for
the transobturator route.
In fact, very few studies have assessed medium- to long-
term outcomes of the TVT-O procedure
[7–12]. In some of
these studies, women with OAB symptoms or with
urodynamically proven DO were included, which can
reduce the reliability of the results
[8,9,12] .The available
data on the efficacy and adverse effects of transobturator
MUS over 5-yr follow-up are limited at two studies.
Athanasiou et al
[13]reported 7-yr objective and subjective
cure rates of 81% and 83%, respectively. The slightly lower
cure rates could be due to the fact that in their retrospective
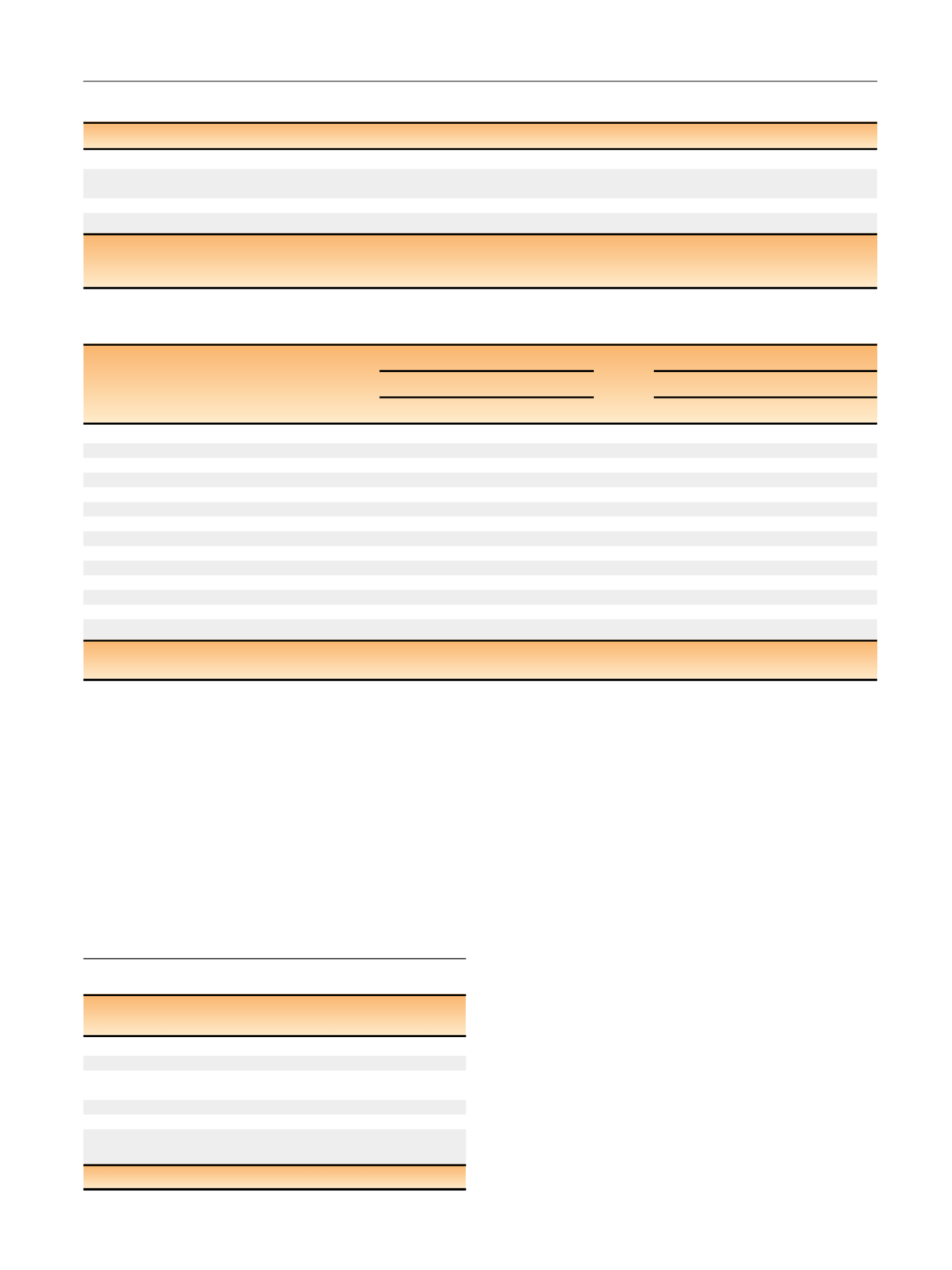
Table 5 – Clavien-Dindo classification of long-term complications
Complication
Patients
(
n
= 160)
Action
Clavien 1
Persistence of groin pain, no. (%)
1 (0.6)
Observation
Persistence of voiding
dysfunction, no. (%)
1 (0.6)
Observation
Clavien 2
De novo overactive bladder, no. (%)
23 (14)
Antimuscarinics
De novo dyspareunia, no. (%)
4/9
2 * (4.3)
Local estrogenic
therapy
*
Patients sexually active at 10 yr.
Table 3 – Subjective outcome scores at 5 and 10 yr after tension-free vaginal tape–obturator
Baseline
5 yr
10 yr
p
value
ICIQ-SF, median (IQR)
17 (16–17)
0 (0–2)
0 (0–2)
<
0.000
1 *‘‘Very much better’’ or ‘‘much better’’ on PGI-I, no./total no. (%)
155/168 (92)
155/168 (92)
Patient satisfaction scale, median (IQR)
10 (8–10)
10 (8–10)
80% reduction in UDI score, no./total no. (%)
154/168 (92)
153/168 (91)
ICIQ-SF = International Consultation on Incontinence Questionnaire–Short Form; IQR = interquartile range; PGI-I = Patient Global Impression of Improvement;
UDI = Urogenital Distress Inventory.
*
One-way analysis of variance.
Table 4 – Univariable analysis of variables potentially involved in the risk of failure of tension-free vaginal tape-obturator at 10 yr
Variable
Subjective failure
Objective failure
Univariable analysi
s aUnivariable analysi
s aHazard ratio (95% CI)
p
value
Hazard ratio (95% CI)
p
value
Elderly, age 65 yr
0.41 (0.23–1.14)
0.13
2.12 (0.84–5.73)
0.2
Obese, BMI 30 kg/m
2
1.84 (1.13–5.12)
0.05
1.53 (0.52–4.61)
0.5
2 vaginal deliveries
0.42 (0.11–1.23)
0.3
0.80 (0.31–2.34)
0.8
Macrosome, 4000 g
0.71 (0.15–3.14)
0.6
0.63 (0.12–2.83)
0.5
Operative delivery
2.12 (0.63–7.62)
0.2
0.53 (0.07–3.91)
0.6
Cesarean delivery
0.04 (0.01–75.6)
0.5
0.04 (0.01–41.4)
0.3
Menopausal
0.23 (0.03–1.70)
0.17
2.92 (0.34–4.33)
0.4
HRT
1.53 (0.52–4.31)
0.4
1.23 (0.43–3.82)
0.7
Recurrent UTI
1.44 (0.45–4.20)
0.5
1.51 (0.50–4.63)
0.5
Smoking habit
0.45 (0.14–1.63)
0.2
2.32 (0.83–7.21)
0.14
Previous anti-incontinence procedures
5.34 (2.61–11.9)
0.009
2.74 (1.64–10.7)
0.009
Surgeon’s skill, resident vs expert
0.41 (0.06–3.33)
0.4
0.52 (0.06–3.50)
0.5
Urethral hypermobility, Q-tip test result
>
30
8
1.32 (0.24–10.23)
0.8
1.41 (0.03–2.12)
0.3
VLPP
<
60 cm H
2
O
1.31 (0.31–5.81)
0.7
2.62 (0.81–3.42)
0.09
BMI = body mass index; CI = confidence interval; HRT = hormone replacement therapy; UTI = urinary tract infection; VLPP = Valsalva leak-point pressure.
a
Univariate Cox proportional hazard model
E U R O P E A N U R O L O G Y 7 1 ( 2 0 1 7 ) 6 7 4 – 6 7 9
677
















